Editor's Note: This text is a transcript of the course, Sleep: The Challenge of Aging, presented by Teresa Fair-field, OTD, OTR/L.
Learning Objectives
After this course, participants will be able to:
- Identify differences between typical sleep patterns and problem sleep
- Identify confounding factors affecting sleep hygiene in the elderly
- List appropriate responses to sleep problems in the elderly population
Introduction and Overview
I love talking about the topic of sleep. It is something that everybody can benefit from on a personal or professional basis, so I hope everyone takes away something today that benefits them in a broad sense. Our learning outcomes for today are that you will be able to identify the differences between typical sleep patterns or expected sleep disruptions and problematic sleep, identify the confounding factors that affect sleep hygiene, particularly in the elderly population, and then list appropriate responses for those sleep problems. Toward the end of the course, we will also talk about how you can participate in supporting a sleep culture at the facilities where you may work.
Typical Sleep and Sleep Architecture
How Much Sleep Should We Get?
Let's begin by talking about what typical sleep is. Sleep researchers call this sleep architecture. Here is what we should be getting throughout the lifespan, according to the National Sleep Foundation:
- Newborns (0-3 months): Sleep range narrowed to 14-17 hours each day (previously, 12-18)
- Infants (4-11 months): Sleep range widened two hours to 12-15 hours (previously, 14-15)
- Toddlers (1-2 years): Sleep range widened by one hour to 11-14 hours (previously, 12-14)
- Preschoolers (3-5): Sleep range widened by one hour to 10-13 hours (previously, 11-13)
- School age children (6-13): Sleep range widened by one hour to 9-11 hours (previously, 10-11)
- Teenagers (14-17): Sleep range widened by one hour to 8-10 hours (previously, 8.5-9.5)
- Younger adults (18-25): Sleep range is 7-9 hours (new category)
- Adults (26-64): No change with 7-9 hours
- Older adults (65+): Sleep range is 7-8 hours (new category)
The National Sleep Foundation’s website has a printable infographic that may be useful for you to disseminate or hang up at work. One thing to note is that the recommendations have changed due to recent advances in sleep science. The recommended hours of sleep shown above are from a 2017 study, so it is quite up to date. The latest research has resulted in subtle changes to our understanding of the amount of sleep necessary at every stage of life. New findings show that there is actually a narrowed recommended sleep range in the smallest newborns; previously it was 12 to 18 hours, and now it is actually more like 14 to 17 hours. For infants 4 to 11 months old, the recommended range has widened to 12 to 15 hours, a two-hour difference in the lower number. Similarly, the recommended range of sleep hours for toddlers, preschoolers, school-aged children, and teenagers has widened as well, by about one hour each. Interestingly, adults have now been divided into three groups, with the new age categories of younger adults (age 18-25), adults (age 26-64), and older adults (age 65+). Previous versions of these recommendations did not acknowledge any variation in sleep needs for adults age 18 and up, but we now know that that is not true. For adults, the range is still 7-9 hours, and it is the same for younger adults; for the new “older adults” category, the expected range is narrowed to between 7 and 8 hours of sleep.
How Much Sleep Do We Actually Get? The Sleep Health Index®
While the ranges have not changed dramatically, our understanding of the sleep process in those adult age ranges has changed, and that is what we will be discussing today. In this 2017 study in the peer-reviewed flagship journal of the National Sleep Foundation, Sleep Health, they described results from a 12-item survey tool called the Sleep Health Index. This tool was developed in 2014 and then used over the next two years to survey over 2500 adult Americans. Using factor analysis, the researchers identified three different domains of sleep: sleep quality, sleep duration, and disordered sleep. The index provides a score on a scale of 0-100 in each of those subareas, and then an overall total score. The tool researchers then used regression analysis to determine what independent predictors of sleep are.
These two years of research revealed that the average American adult reported receiving about 7 hours and 36 minutes per night, which is well within the recommendation for that age group. You will see that on workdays, the average bedtime is 10:55 p.m. and the average wake time is 6:38 a.m., but the average sleep time is 40 minutes longer than that on non-workdays. So, not surprisingly, we are getting less sleep on days that we work, relative to days we are not working. Also not surprisingly, young adults between ages 18 and 29 reported the latest bedtimes. In this particular study, duration of sleep did not differ between men and women.
Population Surveyed
You may wonder who these people are that are sleeping an average of 7 hours and 36 minutes per night because you, in fact, may be getting substantially less. The population surveyed was fairly evenly distributed between men and women, with 48% of survey takers being men, and 52% being women. Age distribution was also fairly even, as was income across a full range. Of note, older ages did predict disordered sleep, but was not correlated with sleep quality or duration in this study. As we will discuss, disordered sleep means sleep that is broken up across the day, rather than what we call consolidated sleep, which is a single sleep set when we get all of our hours.
Only 57% of this sample was employed, so that may be an indicator of how much sleep they are getting. The remainder were categorized as unemployed, but it should be noted that this group included students, retired people, those on disability, and stay-at-home parents, in addition to individuals that were fully unemployed. The regression model indicated that employment did negatively affect sleep duration (i.e., the length of time spent sleeping), but it did not affect sleep quality and did not contribute to disordered sleep. That is, having either a part-time or full-time job simply meant that subjects spent less time in bed.
Racial representation is also a critical factor in analyzing sleep. There is a growing body of literature describing the impact of racial and socioeconomic disparities on sleep, including the effects of neighborhood disadvantage on the sleep environment and the impact of psychosocial and occupational stressors - even racial battle fatigue - and their effect on sleep processes. Please see the references at the end of the course for those resources and findings.
The study also included individuals with an identified disability, which directly impacted sleep. So, the study looked at typical sleep across a very broad adult population, although it should be noted that the tool was not designed to be administered to a pediatric population.
It is important to know that prior to this very recent study and tool, there was not a valid and reliable research survey to determine the state of sleep health in the U.S. We can hope that now that there is such a tool, the road will open for additional studies that can focus on unique issues affecting sleep in minority populations and in the aging.
What is Normal Sleep Architecture?
You probably know that rapid eye movement (REM) and non-REM sleep make up a normal sleep cycle, but what do these cycles look like? How many times do we cycle through? And what happens when we do not? How does sleep get disrupted or disorganized?
Graphics such as Figure 1 below may look familiar to you if you have used a fitness wristband with a sleep app that can track your nocturnal movements and heart rate to give an indication of your sleep trends.
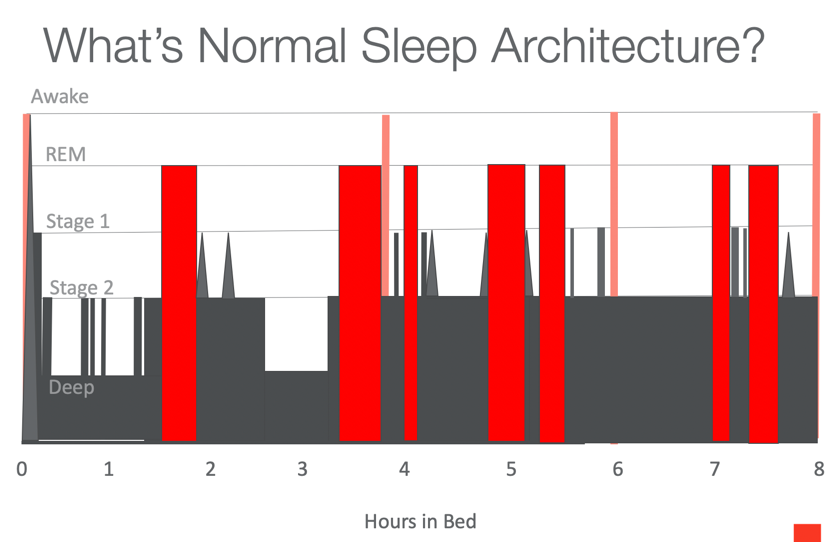
Figure 1. Normal sleep architecture.
Let's take a closer look at this particular graphic. You see at the bottom that the X-axis is hours in bed. The Y-axis indicates stages of sleep: Awake, REM, Stage 1, Stage 2, and Deep.
Wakefulness is at the very top, so anytime the bar comes to the top, it represents an awake state. In normal sleep architecture, you are in a state of wakefulness, of course, at the beginning and the end of your sleep cycle. But you also see wakefulness occurring a couple of times as you actually wake up before ending your sleep cycle at the end of the night. Those wakeful states occur after about four hours in bed and about six hours in bed. It varies, but this rise to wakefulness is a normal part of sleep architecture. You may drop back down to deep sleep if you are undisturbed, or you may actually come to full wakefulness if there is a sleep disorder or a sleep disruption in the cycle. You may notice anecdotally that as you talk to people about their night’s sleep, you commonly hear, “I only got four hours of sleep” or “I only got six hours of sleep.” You rarely hear, “I only got three hours of sleep,” and that is because wakefulness does not tend to occur around this third hour; around that time, you tend to be in a stage of very deep sleep.
The next thing I would like you to notice is what happens when you are first falling asleep, at the front end of the graph, after zero to one hour in bed. You see that the line dropping down from wakefulness waterfalls very quickly through all of these stages - Stage 1, Stage 2, and then into deep sleep - in just a matter of minutes. This is a very quick falling asleep into deep sleep phase.
Now, let's discuss those stages of sleep. All three levels, Stage 1, Stage 2, and Deep, are considered non-REM. REM periods are the red bars in this graph that recur across the cycle, that rise up to where “REM” is written on the Y-axis. We do not get to REM sleep until we have been asleep for close to two hours.
Think about your own sleep as we talk about this chart, because we will assume you are a normal pain free sleeper. It is helpful to compare your own experience as you hear this information.
In non-REM Stage 1, at the beginning of your sleep cycle, your eyes are heavy and closed, but you may not feel as if you are asleep. You do not spend too much time in this stage before dropping down into Stage 2, which is when you feel your muscles both contract and relax, and your heart rate and your body temperature go down. Again, you are in Stage 2 for just a few moments until you drop down into stage three sleep or deep sleep. In deep sleep, you are so deeply asleep that you are disoriented if awakened. It is the deepest stage of sleep that you will experience. Looking at the graphic, you can see that you drop into that deep sleep fairly quickly. You are in deep sleep for most of the first two hours of your sleep cycle except for a few bursts back into Stage 2 sleep. You may notice that those Stage 2 spikes are when your body jumps or jerks suddenly. You go back to deep sleep for a portion of time around the three to three and a half hours in bed mark. If you look at the deep sleep bars, you will notice that they only occur in the first half of the entire sleep cycle, and that after about three and a half hours in bed, the deep sleep stage disappears entirely. We do not get down to deep sleep again later in the night. In other words, in those years I spent waiting for five hours before sneaking presents under the tree for my child, he was much more likely to wake up then than if I had done it shortly after he had fallen asleep.
Now let's talk about REM sleep, which first appears as the red bar that you see just inside of two hours - about 90 minutes or so after you fall asleep. Another thing you notice about those bars is that the width of them is variable. But most REM cycles are about 10 minutes long; some a little less, some a little more. REM, as you may be aware, is actually a very active sleep phase, in which not only are your eyes moving rapidly, but your heart rate and your respiration rate increase from what they were. These periods of REM are sprinkled throughout the sleep cycle, but do not begin until you have been asleep for almost two hours. You will also notice that none of those REM cycles occur just before or after deep sleep; they typically occur when you are already at Stage 2, though it is possible they may occur before or after Stage 1 sleep. This is something that we will go on to discuss relative to the sleep environment, so I want you to keep it in mind.
The takeaway message from this slide on normal sleep architecture is that in normal sleep, a deep sleep stage occurs in the earlier half of the sleep cycle, disappears, and does not recur in the latter half of the night. Also, in addition to when you first lie down and then finally get up, wakefulness occurs at regular intervals throughout the night; typically, this occurs at the four- and six-hour points, but most sleepers do not fully awaken during these middle-of-the-night times unless sleep is disrupted. The other thing to notice is that light sleep punctuates the entire sleep cycle, even in normal sleep.
By the way, if you are wondering about the accuracy of a consumer wearable device in measuring your sleep, there is research to indicate that those devices are fairly accurate for basic consumer purposes. They are actually much better at measuring the sleep cycle than they are at measuring calories burned because there are fewer confounding variables affecting your sleep movement. But they do tend to overestimate sleep duration by some amount – typically between 24 and 67 minutes - compared to an accelerometer device used in sleep research. Nonetheless, most consumers find that it is an adequate indicator for their home use.
Sleep Process Factors
Now, we are going to discuss the two sleep process factors, Process S and Process C, as well as dim light melatonin onset (DLMO) and the role of melatonin in the body.
Two-Process Sleep Model
In this two-process model, sleep scientists have identified Process S, which is sleep pressure build-up, and Process C, which is our circadian rhythm. As you may know both affect and influence sleep.
Process S. In Process S, what is called sleep pressure, or the need for sleep, is built up over hours of wakefulness. At the very beginning of the first sleep phase, sleep pressure is very high, because presumably, you have been awake for a number of hours. That sleep pressure diminishes as sleep occurs and you start to pay back that sleep deficit. If you are disrupted later on in your sleep process - recall those cycles of wakefulness from our chart that occur at four and six hours of sleep - you may not get back to your sleep cycle again. That may happen for a variety of reasons, but one reason is that after the several hours of sleep that you did get, you may no longer have adequate sleep pressure built up to return to a sleep state.
Process C. Process C is the circadian rhythm that determines the sleep/wake rhythm. We see that it first emerges in newborns at about three months of age. Prior to 12 weeks, the very young newborn tends to have equal phases of sleeping and wakefulness across 24 hours. Another change occurs in middle childhood when you see sleep preferences emerging for being either a “morning person” or a “night owl.” And then, there is another shift in puberty as DLMO, or dim light melatonin onset, causes a one- to two-hour shift in both bedtime and morning arousal. However, while bedtimes do shift later, adolescents are generally unable to shift their wakeup time to one to two hours later; that is when an adolescent sleep deficit pattern starts to emerge. We are starting to see some school districts pay attention to the research and shift their school start times to later in the morning, in order to accommodate those biological factors for children of that age. Some of you who are parents with children in school may begin to hear about that.
In general, this Process C is regulated by zeitgebers, which comes from a German word meaning “time givers.” Zeitgebers include daylight, darkness, and daily routines such as mealtimes, and social activities, and self-care routines. Habituation of these zeitgebers prompts the release of melatonin. Let’s look at that more closely.
Dim Light Melatonin Onset
Melatonin is a naturally occurring hormone secreted by the pineal gland, and it is the most essential hormone affecting the sleep/wake cycle. Its release is triggered in part by those zeitgebers that we just discussed, one of which is the impact of both natural and artificial light. When our bodies are exposed to the dimming of available light - something that occurred for millennia prior to the advent of electricity - it triggers the release of melatonin, which prompts the body to begin readiness for sleep. Of course, our use of lightbulbs and all kinds of screens (e.g., phones, televisions) has interrupted many of these processes. I am sure I do not need to reiterate that dimming your screens and avoiding them all together at night is an important part of Process C. What may be surprising, though, is that melatonin begins to be released about two hours prior to the onset of sleep, so if you are using light blockers or dimmers, they need to be activated at least two hours before your planned bedtime. In addition, you need to avoid screens that are not dimmed during that period of time, in order for the melatonin release to be maximally effective. Many studies in both research journals and the popular press discuss the effects of artificial light and blue screen technology on the release of natural melatonin. Now, if the body has been exposed to daytime light during the day that dims as we move toward sleep, the average onset of sleep - that is, the amount of time that it takes for people to fall asleep from the moment they hit the pillow - is about 20 minutes. If they have been exposed even to blue filtered light, such as a phone with a blue blocker, that number could go up to about 30 minutes. And if they are exposed to bright blue enhanced lights, such as exist on unfiltered smartphones, studies have shown participants were still awake anywhere from 30 to nearly 80 minutes after their heads hit the pillow. That is well over an hour where they were struggling to get to sleep. Of course, since we tend to be impatient as we are staring at the ceiling, if we keep the phone by the bed and it is taking us an hour to get to sleep, chances are we will reach for that phone again to entertain ourselves while we are waiting. That, of course, compounds the problem.
Sleep Changes in the Elderly
Let's summarize the sleep changes that we see in the elderly. When discussing the Sleep Index earlier, we said that the amount of sleep - the sleep duration - is not much affected by aging. Still, we know that even if elderly individuals are sleeping the ideal duration, they do show sleep cycle changes. One such change is that they spend less time in Stage 3 sleep. Recall from our sleep architecture slide that that is the deepest phase of sleep. An elderly individual may never get down to that level of deep sleep, which is actually the most restorative phase of sleep. They spend less time in those deep phases, and they also have reduced sleep pressure. This is because if there is disordered sleep, and sleep is occurring for individuals in bits and pieces over the course of the day, they never have the opportunity to build up the sleep pressure that will produce a long cycle of sleep during the night. In aging individuals, there is also reduced strength of the circadian signal, as well as a reduction in melatonin production and a delay in its delivery. Keep in mind that the elderly may not be having the same exposure to natural light and dark during the day, and that also will impact the effect of the circadian signal.
We know that they are spending more time in Stage 1 sleep, the very lightest phase of sleep, which means that sleep is shallower and more disrupted over the course of the sleep cycle. Elder individuals are also more sensitive to subtle changes in the sleep environment, something that becomes very important when we look at the sleep culture inside of facilities. Lastly, dehydration, a not-uncommon issue in the elderly, may also be a factor that disrupts sleep.
Sleep Problems: Parasomnias
Now let's take a look at normal sleep compared to abnormal sleep, which includes parasomnias and dyssomnias. We are going to talk about parasomnias first. Although they are rare, they are what we think of when we talk about disorders of sleep, because they are what we hear about in movies and stories.
Parasomnias occur at the transition between sleep and wakefulness, which results in an altered psychological state. They tend to occur when an individual’s sleep phase is partially disrupted. Recall that these disruptions are typically clustered in the first part of the sleep cycle, so we tend to see more parasomnia behaviors occurring in the first part of the night.
Parasomnias include issues like night terrors, nightmares, sleepwalking, and the like. Night terrors may be familiar to you; since they occur in the earlier part of the night, caregivers are usually still milling around when a night terror strikes. Caregivers tend to attempt to interact and console the person who is exhibiting an autonomic nervous system response, but that person is visibly in “fight or flight” mode. If returned to bed, they tend to have amnesia for the episode; that is, they do not remember it even occurring. There is a genetic component to parasomnias, and they tend to occur in a fairly small percentage of the population, about 1-7% of children and about 2% of adults.
Sleepwalking episodes are usually short and can occur as a repetitive motor behavior, such as picking or pacing. But you have probably heard about more unusual sleepwalking stories where a sleepwalker will exit the home or be found in the neighbor’s yard. Sleepwalking episodes typically last less than 15 minutes, but episodes of up to an hour have been reported. If awakened, the person who is sleepwalking may be combative or violent if you attempt to interact with him. Up to 40% of children have had one sleepwalking episode in their lifetimes, and about 2-3% of children have more than one a month. Interestingly, the same number of adults continue to sleepwalk later in the lifespan.
The best response to both sleepwalking and night terrors is to keep the person asleep or in their existing state, to minimize the interaction, and steer her back to bed without attempting to wake her or have her process the incident. Understand that they are having a parasomnia, and so sleep - not wakefulness - is the cure. That is often where we make a mistake as caregivers; we think that rousing them into wakefulness will disrupt the activity, but actually, returning to sleep without interaction is the cure.
Therefore, steering them back to a safe sleeping place is the surest strategy.
Confusional Arousals
Confusional arousals are quite common. These are also partial arousals from sleep, like the parasomnias we just discussed, but these actually occur during the waking up phase, whereas parasomnias are early-night sleep phase disorders. Here, the individual requires a longer than expected time to become alert. Confusional arousal is quite common in both children and older adults, as well as in the sleep-deprived. Since this is somebody coming into wakefulness, the best thing to do is to keep him safe and to have minimal interaction and not attempt to force wakefulness. The individual needs to settle into the environment and naturally come to a fully alert state when he is ready. This might sound familiar to some of you who have had grumpy interactions with people who have difficulty reentering wakefulness during the morning.
Unusual Parasomnias
There are a handful of other parasomnias, such as sleep-related eating disorders where individuals consume what are typically highly caloric or forbidden foods, or strange foods, while in a sleepwalking state. There is a REM sleep behavior disorder in which individuals can be violent and combative during REM sleep. These are fascinating case studies, but largely outside of the scope of this course. It is good to keep in mind, if you see unusual behavior in a child or older adult and it is paired with what might be considered diminished alertness, remember that it could be a result of a sleep disorder, and it will be important to mention to the team.
Sleep Problems: Dyssomnias
The word dyssomnia comes from "dys" meaning dysfunction, and "somnia" meaning sleep, so dyssomnia is a generalized difficulty with either falling asleep or staying asleep. People with dyssomnias have either poor quality or quantity of sleep or poor organization of sleep relative to the normal sleep cycle that we saw earlier. As a result of dyssomnia, a person may have excessive daytime sleepiness, of course, but could also have cognitive and behavioral changes that are correctable with sleep improvement. As speech and language professionals focused on cognition, these are some things to keep in mind when you are doing those cognitive assessments; take a look at how your patients are sleeping, as a factor related to daytime cognition. As a result, sleep should always be discussed by the entire team when you are considering factors that affect a resident or client’s safety or performance.
Prevalence of Older Adults with Dyssomnias
Several studies have found an increase in sleep problems in older adults, and these tend to be both intrinsic and extrinsic in nature. As we discussed earlier, the National Sleep Foundation determined, using their Sleep Index, that older adults were no different from other adults in either sleep quality or overall duration, but that they had significantly more disordered sleep; that is, sleep was not well organized in the older adult.
In what ways is it disordered? The following are the types of dyssomnias that are prevalent in older adults with difficulty either falling asleep or staying asleep, based on data from 2017. Ninety-four percent reported waking up at least once during the night, and 57% woke up too early in the morning. Insomnia - difficulty falling asleep in the front part of the night - affected 36% of the sample, and a far greater number of women than men. Researchers believe that is likely related to the continuation of hormonal changes in postmenopausal women. And then 27% of the sample subjectively reported feeling as though they just did not get enough sleep.
So, is this a standard sampling of older adults in our residential communities? It probably is, though neurological conditions, such as stroke, acquired brain injury, or dementia are not represented in these numbers; again, these were community dwelling older adults. We can expect that in our treatment populations, these numbers would, in fact, be far higher. In this sample, 99% of respondents had one or more chronic medical conditions, such as hypertension, osteoporosis, diabetes, or renal disease, whereas less than 2% of the sample had a diagnosed condition of sleep apnea. That is something we will talk about shortly.
Extrinsic vs Intrinsic Factors
Dyssomnias can be further characterized as those that are extrinsic, or occurring outside of the body, versus intrinsic, which are related to the function of the body.
Extrinsic factors include room temperature, ambient noise or light, stress, and sleep behaviors (often called sleep hygiene). Examples of intrinsic factors - inside of the body - are pain, respiration, sleep apnea, internal regulation, possible seizure activity and restless leg syndrome, which we will talk more about in a moment.
Extrinsic Factors
Room temperature/layers. One of the easiest extrinsic factors to address in modern society is room temperature. It has been identified that ambient room temperature between 60 and 67 degrees at night is the most conducive to both falling asleep and staying asleep. However, we know that elderly people tend to keep warmer home/bedroom environments as a matter of preference, due to more sedentary lifestyles, issues of circulation, etc. As caregivers, if we support residents in dropping their thermostat temperature at night, it may positively affect their sleep quality. Research does show that dropping core body temperature at the REM sleep cycle point significantly impacts sleep duration and quality, particularly in elderly sleepers. We will look more at core body temperature when we discuss internal regulation, which is an intrinsic factor, but this is one way that the extrinsic factor of room temperature, is related to an intrinsic factor. According to that study, the elderly population is more sensitive to room temperature changes affecting their sleep cycle, which causes more frequent waking and can decrease REM sleep. As you recall, the elderly spend more time in lighter stages of sleep. They tend to wake up because their body temperature does not have the opportunity to drop, and dropping body temperature is what prompts deeper levels of sleep to occur.
Clothing worn to bed also impacts thermal regulation. It is discussed here because the clothing you wear on the outside of the body is an extrinsic factor that you can control. However, it is often a matter of strong personal preference and can be a cultural one as well, so changing one's bedtime apparel may not be as easy to do as changing the temperature mechanically in the room environment. The layers or warmth of clothing the individual wears to bed and the amount of blankets and covers on the bed may affect how they are able to externally regulate their nighttime body temperature. That cocoon warmth does, in fact, help individuals fall asleep initially; however, the body's impaired ability to lower its temperature, if it is covered in clothes and covers, can actually cause wakefulness and prevent subsequently moving into Stage 2 and deeper sleep.
So, lowering that thermostat later in the evening after the person has retired, and adjusting that setting based on how many clothes and layers she wore to bed, can have a positive effect and reduce nighttime wakefulness due to a too-warm condition. Remember, some of those spikes into the awake state for yourselves or your loved ones may be occurring when you are too hot and you throw the covers off. Those instances can cause full wakefulness rather than letting the individual drop back into a deeper level of sleep.
Ambient noise. Ambient noise is something we are going to talk about here, even though your ability to control it as a daytime worker may be limited. If you come to the team armed with this information, you can advocate for your residential communities to be watchful of nighttime noise. Research shows that a loudness level of 40 decibels or lower is recommended for optimal sleep, and that is equivalent to a quiet evening street in a residential neighborhood. In comparison, a quiet rural area is about 30 decibels, and a conversation in the home is about 50 decibels. Most vacuum cleaners are about 70 decibels, even the expensive ones, so chances are that our heavy-duty facility vacuums are far above that. Considering that the deepest sleep occurs in the front part of the evening, it makes more sense, if staff is vacuuming at night, to have them run the vacuum in the hours shortly after the residents have gone to bed. At this time, the residents’ sleep pressure will be at its highest and their sleep cycle will be at the deepest levels, so they will be less likely to be disrupted. Yet how often do we hear about staff waiting until the wee hours of the morning to complete their vacuuming in the halls?
Ambient light. It is not just city dwellers that are affected by ambient light coming into the bedroom. Facility residents might be affected by a parking lot street lamp, for example, or streetlights on adjacent streets as well, especially as residential communities are converting their streetlights to the intensely bright LED bulbs. Therefore, it is important to check whether window coverings are adequate to establish room darkness, either by asking the resident if they are kept up by light, or by communicating with the nighttime staff. If it appears to be a problem that window coverings cannot fix, then facility administration can request that a shield be placed on city streetlamps, for example, or on their own parking lot lights.
Nightlights are fine, since they tend to be low wattage and located near the floor, and of course, they are essential for resident safety. A dimmed lamp at eye level or overhead is less desirable, since it can cause increased wakefulness at those normal waking intervals. The team will need to carefully balance resident safety with their sleep needs.
Ambient light also refers to the amount of light exposure that a resident receives as bedtime nears. Think back to our melatonin slide; residents that use electronic devices, as they often do to combat loneliness or boredom in the evening hours, may not be aware of the effects of blue light, which can delay sleep. Checking that function for our elders’ devices is important, as well. This is yet another demonstration of how an extrinsic factor can impact sleep quality.
Stress/psychosocial factors. This is something we can all relate to, to some degree, but it uniquely affects our elder population. Stress leads to hyperarousal or perseveration, which both delay falling asleep as well as causing you to become fully awake at those normal middle of the night times and preventing you from dropping back into a deeper sleep cycle. If the person is unable to get back to sleep, having awakened during one of those middle of the night points, it may be due to perseverative thoughts. In addition, psychosocial factors that have been recorded specifically in the elderly are increased bereavement and grief in the nighttime hours, and fear of dying during sleep.
Any number of team members can explore these causes of nighttime stress, whether it is a single issue or a collection of concerns. Discussing such issues with the resident during your daytime treatment sessions could be an important method of revealing what may be impacting their sleep. You may have the rapport with the resident to bring some of these issues to light, and then you can pass the information on to other team members as well.
Many mindfulness techniques are available that the individual can be taught to perform while trying to get to sleep or return to sleep. Teaching those strategies during daytime therapy hours, and asking for return demonstrations by the resident, can improve independent performance of them at night when they are most needed. A log of these activities at bedside can be helpful, or a recording device that allows an individual to record and express their thoughts. In addition, supplementing your speech therapy program with a physical therapy or wellness program if they are not already involved, or an occupational therapy referral if they are not already involved, or a mental health referral may be indicated, as well.
Sleep hygiene. Sleep behaviors, which is also called sleep hygiene, refers to those habits that we have and how they affect sleep. Educating our residents on how these habits impact sleep, and providing ways for them to engage and participate in healthy habits, can dramatically improve their sleep. That includes limiting any daytime naps to about 30 minutes and avoiding stimulants and depressants, such as alcohol, near bedtime. As we are moving them towards greater wellness, we should also make them aware of the recommendation to stop drinking coffee or other caffeine about four to six hours before bedtime. So, for people with an early bedtime, that means that they should probably not have coffee after lunch; they will need to watch their consumption of coffee in the afternoon hours.
Nicotine and alcohol cessation is, of course, a good idea for health overall, but in addition, both of those can significantly impact sleep cycles. An individual may believe that those things will help her get to sleep, and it may be true that they help her fall asleep initially, but then they can cause wakefulness later on in the sleep cycle.
Daytime exercise is a powerful tool to improve both sleep quality and duration. Exercise also needs to be completed about four hours before bedtime, so for those of us that tend to work out after our work hours, it may be impacting our body's ability to quiet down for sleep. An individual should also avoid heavy foods at night since digestion can delay sleep onset.
The individual should get adequate daylight during the day to stimulate that melatonin onset, as we have discussed. This can be accomplished by outside or courtyard time, adequate exposure to windows and natural light. We may need to open up those closed blinds we see in so many rooms, in both shared and private room spaces. Often, residents that are in their rooms for much of the day also keep their windows covered during that time, and that is detrimental to the body clock as well as mood and engagement. Again, the education and support of the therapy team is critical here.
One thing to be aware of is what sleep researchers call the wake maintenance zone. Activity, but not exercise, in the few hours before bedtime is essential to having good nighttime sleep. In studies, older adults were accumulating more sleep than younger participants in the hour or two leading up to bedtime; however, these are the individuals that are falling asleep in the hallways at four o'clock. We need to make our residential environments aware that residents need to maintain that wake maintenance zone in the later afternoon, pre-dinner hours to ensure that they have optimal sleep pressure at bedtime. If we think about the way activities are staggered in our facilities, they usually tend to be scheduled in mid-morning and early afternoon, and then those activity schedules tend to drop off right around the time we need those residents to stay awake in order to have a good night’s sleep.
Intrinsic Factors
Pain. Thinking back to the intrinsic factors affecting sleep that we listed earlier, chronic pain and discomfort in positioning are the most commonly cited reasons for poor sleep in older adults. In our treatment population, they most certainly are significant factors. Let’s look at how those issues affecting the older adult can impact sleep, and how we can mitigate them.
In a very large (n=3732) study of Japanese people over age 65, 68% of that sample complained of bodily pain affecting sleep. There is clearly a high percentage of pain in the elderly population. Those who reported higher rates of pain also reported taking longer to fall asleep, more frequent awakening, and poorer sleep consolidation than other subjects.
The mechanism affecting sleep is unclear; there are a number of confounding variables related to pain, but it is understood that pain increases the level of arousal, which then interferes with the body quieting down for sleep. Furthermore, pain medications, or medications for underlying conditions causing pain, may be affecting the sleep cycle as a side effect.
Typically, non-pharmacological interventions, such as imagery training or progressive muscle relaxation, are recommended. These can be provided by the therapy team or a wellness program. A sleep restriction program may be devised by the medical team if sleep is delayed by three or more hours, or two to three hours on successive nights. We will discuss that in a later slide.
Respiration-related factors. Now that we are moving into respiration, I want to establish a background of understanding. Apnea is any cessation of breathing lasting at least 10 seconds, during which there is no respiratory effort.
There are three types of apnea: central, obstructive, and mixed. In central apnea, you see an impaired neurological signal in which the brain is not effectively triggering respiration. With obstructive apnea, you see a mechanical problem interfering with respiration; this might be due to upper airway issues such as tongue positioning, soft palate or pharyngeal collapse. In mixed apnea, aspects of both are present.
Hypopnea, on the other hand, comes from the root of "hypo," or “below.” It is defined as slow or shallow breathing that is inefficient and causes desaturation of at least 4% or greater.
Sleep-disordered breathing (SDB). With that background, let’s discuss the significant aspects of respiration affecting the elderly. Sleep-disordered breathing refers to the general disruption of breathing during sleep in a large portion of the elderly. Sleep-disordered breathing is directly dependent on age and we see prevalence as high as 70% in the elderly, depending on the population being studied. In one study, 44% of adults over 65 were recorded as having at least 20 events per hour, which is a significant loss of oxygen. Of significant interest, there is evidence of a direct correlation between sleep-disordered breathing and dementia in individuals younger than 80. At age 80, there are some other factors that start to affect cognition, of course. But in those younger than 80, the higher the severity of sleep-disordered breathing - meaning the more episodes per hour - the more severe the cognitive decline and effects of dementia. Once sleep-disordered breathing has been identified, continuous positive airway pressure (CPAP) is recommended to reduce the number of events per hour. We will discuss CPAP a little further on.
Obstructive sleep apnea. I know you are aware of sleep apnea, but hopefully, this will expand upon some of your understanding. The most common factors seen in obstructive sleep apnea are obesity, male gender, age, and heredity. It tends to be undetected or under-diagnosed in elderly women, in particular. This is particularly interesting given the prior slide where we discussed the relationship between respiration and dementia because we tend to see higher levels of dementia in women, and fewer women have their sleep apneas identified. This is an area where research is expanding and you might want to consider getting your elderly clients and family members into a sleep study, particularly the women. I am already noticing this trend in research on the west coast.
Another thing to consider is the finding that obesity is no longer predictive of sleep apnea once an individual reaches their 70s and 80s, if it has not already been diagnosed at younger ages. That is because across body types and body mass index (BMI), we see what is described as an age-dependent loss of pharyngeal motor units. There is a study currently underway that is evaluating the effectiveness of an overall strength training program on the performance of those motor units. That could be a potentially exciting finding. But the takeaway message is that until those results come in, you just will not find a downside to an appropriately administered fitness program for your elderly clients, because exercise and sleep are so closely associated.
Internal regulation. As promised earlier, here we are, discussing internal regulation again, and thermoregulation in particular. We already talked about completing exercise well before bedtime to allow that core body temperature to drop back down to baseline. But let's also look at what naturally occurs in the typical sleep cycle. Again, your body's drop in core temperature actually prompts the body to enter Stage 2 sleep, and then the core temperature comes up again at the end of the sleep cycle to stimulate waking. This is in a full and typical sleep cycle in which the individual is not awakened by various other events.
Periodic limb movement disorder (PLMD or PLMS). PLMS is not quite the same as restless leg syndrome. It is actually twice as common and can co-occur with restless leg syndrome. The difference between the two is that periodic limb movement disorder occurs when the individual is asleep, whereas restless leg occurs when the person is trying to fall asleep but remains awake. Treatment for the condition is standard sleep hygiene; in addition, massage and foot wraps at bedtime have been found to be somewhat effective, per the literature. Overall wellness and fitness programs can help alleviate occurrence of this condition. Iron supplementation or medications may be used depending on severity, impact, or co-occurring conditions.
Restless leg syndrome. Restless leg is a neurological condition wherein there is an urge to move the legs; it is accompanied by paresthesia, a burning, prickly sensation. This occurs across all ages. Prevalence in the elderly is variable, from 4% to 20% depending on which study you read. Again, this occurs at night when the person is awake and lying down, trying to get to sleep. The sensation is alleviated by movement, making this a major cause of nighttime wandering in our residential communities. The treatment response is the same as we discussed above, with standard sleep hygiene, massage and foot wraps, wellness, and fitness. Supplementation and medication should be discussed with the physician.
Alzheimer’s disease. How does Alzheimer's affect the sleep cycle? Let’s discuss this for a few minutes because we see that the sleep cycle pattern is similar to same-age individuals without Alzheimer's, except the deviations that do occur tend to be more severe. That is, individuals with Alzheimer's spend even less time in REM sleep compared with their same-age peers. There is an even greater disruption in their Process C, the circadian rhythm. They are producing less melatonin than their same-age peers. They have greater body temperature dysregulation. So, some of those external strategies for sleep improvement or environment improvement will be of particular interest for individuals in Alzheimer's units. Incidence varies depending on the study, but generally, about a third of individuals with Alzheimer's have disordered sleep. It can be a significant source of stress for caregivers who then have their hands full during the nighttime, as well as the daytime.
Treatment for the individual is the same, depending on the issues affecting sleep. But sleep hygiene may need to be managed and maintained by the caregiver instead of the individuals themselves. Studies that look at CPAP compliance for sleep apnea or sleep-disordered breathing showed that if it is introduced in the early stages of Alzheimer's and has the opportunity to become habitual in those early stages, then it can be just as successful as it is for individuals without Alzheimer's. Lastly, medications may be recommended, depending on the severity as well as any co-occurring conditions.
Assessment and Treatment Approaches
Sleep logs and sleep diaries are things that we should be initiating use of in our residential communities, and they are very appropriate for speech therapy practitioners to implement. If you make a referral to a sleep medicine specialist, they will give you a recommendation to keep a sleep log before you come back for further workup. Pulse oximetry is helpful as a screening device, but on its own is not a definitive diagnostic tool. Polysomnography (PSG), which is a full sleep study, is the "gold standard" of sleep assessment; it measures brain waves, oxygen, heart rate, respiration, etc. A comprehensive workup would include all of the contributing disease factors, as well as psychosocial, psychiatric, and behavioral factors and also cognition.
Pharmaceutical Approach
We have already talked about sedative hypnotics being discouraged, as they tend to cause adverse side effects such as daytime sedation, motor incoordination, and increased fall risk, in addition to what the individual may already be experiencing. There are some other pharmaceuticals that are recommended, including benzodiazepines and antipsychotics, but they are usually not the right answer and certainly should not be a go-to.
In my experience, among the rehab therapies, speech therapists are often the experts in pharmaceutical interactions and how they impact patients. So, as we are discussing your role on the rehab team addressing sleep, note that it is important to hone your knowledge of how individuals’ medications may affect their sleep cycles.
Melatonin Replacement
In some studies, melatonin replacement has been showing promise, but in Alzheimer's, it also has mixed results, so at present, there is not a definitive answer about evidence-based practice around melatonin supplementation. Those therapies that combine bright light exposure with melatonin supplementation tend to show better response.
CPAP
As we know, CPAP is not curative, but it may reduce the number of respiratory events for an individual. We discussed the fact that if it is introduced early, it may be tolerated by residents both with and without Alzheimer's disease.
Sleep Restriction/Chronotherapy
Sleep restriction is used to change individuals’ sleep pressure and bring them gradually back to a regular bedtime. For an individual that is unable to fall asleep until 2:00 a.m., for example, you would restrict her sleep until her time spent in bed not sleeping is decreased and sleep pressure is increased, to the point where she can move to an 11:00 p.m. bedtime and stick to that. That is something that a physician may recommend.
Shaping a Supportive Sleep Culture
As we close, I want to discuss shaping a supportive “sleep culture.” We talked at length about therapists’ role in providing adequate sensory stimulation and exposure to natural light, and providing activities during the wake maintenance zone, including some sensory wind-down programs that may be meaningful for our individuals and that would prompt those sleep behaviors. All of us on the rehab team can help to promote light exposure during awake hours. Look at later afternoon programming to provide something for individuals during that wake maintenance zone.
If you have a particular interest in the sleep process, step forward as a sleep team champion and form a sleep team in your work environment. We really need to address sleep as something that has an effect on daytime behavior, and discuss as a group the impact of nighttime interactions and cleaning routines. And if the team is seeing behaviors that could be associated with poor sleep, taking that investigative dive into the individual’s sleep should be step one. It is the personal factor upon which all other aspects of performance are based.
I am going to close with questions. The Academy of Sleep Medicine website (https://aasm.org/) is an excellent resource. There are also a number of references on the handout that can be consulted if you are interested in further study. Thank you for your time today.
Questions and Answers
Could you please define sleep pressure again?
Sleep pressure is one of those sleep processes where pressure for sleep is built up over hours of wakefulness. The longer you have been awake, the more sleep pressure or need for sleep builds up in the body.
What is the wake maintenance zone?
The wake maintenance zone is those hours before bedtime sleep in which the individual should be awake. That tends to be around the dinner hour or later afternoon, and we may see residents or elders nodding off when in fact, they need to be kept awake in order to have good nighttime sleep. In other words, the wake maintenance zone is the handful of hours occurring before the point when nighttime sleep is expected to occur.
Can you talk briefly about how poor sleep can contribute to some children being diagnosed with attention-deficit/hyperactivity disorder? Are you able to speak to that?
Absolutely. Although it is a little outside of the scope of this course, I have dabbled in sleep in pediatric populations, as well. There is a large amount of research about how sleep can certainly impact behaviors that are seen in children, if not diagnosis. That is one thing that threads over to our content regarding the elderly, as well. We often look to other issues when we see concerning behaviors, but in fact, perhaps we should be looking to sleep as one of the primary aids that can help ensure the individual has a full set of tools with which to approach their day. This is particularly true for our vulnerable populations, including children and the elderly.
When patients are excessively sleeping during the day, I imagine it affects the sleep pressure. What is your recommendation about the amount of rest people should have during the day?
Again, there was one slide that emphasized that naps should be kept to about half an hour. But it is also true that elders are getting their sleep in chunks throughout the day. It is a balance between keeping them active and awake, and also appreciating their need for increased rest periodically throughout the day. This may occur as a nap, which is completely appropriate. We may not need to intervene where there is not a problem with nighttime sleep; we may only need to intervene when we see behaviors or complaints indicating that sleep is a problem.
Can you explain what nighttime perseveration is?
Perseveration is getting stuck in a thought loop. For our elderly individuals, we may see psychosocial complaints such as loneliness or grief being exacerbated at night, and they can just get cognitively stuck in that space.
Citation:
Fair-Field, T. (2020). Sleep: The Challenge of Aging. SpeechPathology.com, Article 20403. Retrieved from www.speechpathology.com

