From the Desk of Ann Kummer

As the contributing editor of 20Q for speechpathology.com, it has been my pleasure to invite well-known and well-respected clinician-authors to submit 20Q articles for your clinical edification and reading pleasure. This month, it is my turn.
In this edition, I will be answering common questions about resonance disorders and velopharyngeal dysfunction. In particular, I will discuss how these disorders should be evaluated and treated.
Here’s a little about my background: I have worked at Cincinnati Children’s for about 40 years. During most of that time, my clinical work has been focused exclusively on children with cleft palate, various craniofacial conditions, resonance disorders, and VPI. I have been an active member of the Cleft Palate/Craniofacial Team at Cincinnati Children’s and I co-founded our non-cleft VPI Clinic in the early 1980s. In my career, I have evaluated and treated thousands of children and done hundreds of nasopharyngoscopy examinations. I currently teach the craniofacial course at five universities and travel nationally and internationally doing lectures and seminars. In the late 90s, I was inspired to write a book for clinicians on the management of children with clefts and craniofacial conditions. The 4th (and best) edition of this book was just released (Kummer, Cleft Palate and Craniofacial Conditions, Fourth Edition).
Because of the opportunities that I have had to specialize, teach, and learn, I’m really passionate about sharing my knowledge. My goal is to help other SLPs to effectively evaluate, treat, or refer children with structural anomalies that affect speech and/or resonance. As a result, these children will receive the services that they need.
Now...read on, learn and enjoy!
Ann W. Kummer, PhD, CCC-SLP, FASHA
Contributing Editor
Browse the complete collection of 20Q with Ann Kummer CEU articles at www.speechpathology.com/20Q
20Q: Evaluation and Treatment of Speech/Resonance Disorders
and Velopharyngeal Dysfunction
Learning Outcomes
After this course, readers will be able to:
- discuss the types and causes of velopharyngeal dysfunction.
- describe the characteristics of resonance disorders and nasal emission.
- implement effective procedures for evaluation of speech and resonance.
- determine when to provide speech therapy and when to refer the child for physical management.
Normal Velopharyngeal Function and Velopharyngeal Dysfunction
1. Can you start out by describing normal velopharyngeal function?
Sure. The velopharyngeal valve consists of the velum (soft palate), lateral pharyngeal walls, and posterior pharyngeal wall. During the production of oral sounds, the velopharyngeal valve closes in order to direct the sound (from the vocal folds) and airflow (from the lungs) into the oral cavity. The velopharyngeal valve opens for the production of nasal sounds so that the sound energy continues to flow in a superior direction and then through the nasal cavity. During oral speech production, the velum does most of the work by moving in a superior and posterior direction (at a 45 angle) to close against the posterior pharyngeal wall. At the same time, the lateral pharyngeal walls move medially to close against (or in rare cases, behind) the velum so that the entire valve is completely closed.
2. I’ve heard the term “velopharyngeal dysfunction,” and other terms as well. What is the correct term to use?
This is a good question. Historically, many different terms have been used interchangeably. This has caused some confusion and made searching the literature difficult due to multiple keywords, which essentially meant the same thing. More recently there has been a general consensus to use velopharyngeal dysfunction (VPD) as a generic, non-specific term. For more specificity, the term velopharyngeal insufficiency (VPI) is used to describe a condition caused by a structural abnormality (i.e., history of cleft palate, submucous cleft, post-adenoidectomy, etc.). In contrast, velopharyngeal incompetence (VPI) is used to describe a condition caused by a neuromotor condition or disease (i.e., head trauma, stroke, cerebral palsy, neuromuscular disease, etc.). Velopharyngeal incompetence is the cause of several characteristics of dysarthria, including hypernasality, weak consonants, and poor breath support. Finally, velopharyngeal mislearning is the term used to describe a speech sound placement disorder that causes phoneme-specific hypernasality (e.g., ŋ/l, ŋ/ɚ) or phoneme-specific nasal emission (e.g., pharyngeal fricative/one or more sibilants). VPI, regardless of type, requires physical management (not speech therapy), while velopharyngeal mislearning requires speech therapy (not surgery) (Kummer, 2011b; Kummer, Marshall & Wilson, 2015; Kummer, 2020a). (Note that velopharyngeal inadequacy is not included in this more current terminology.)
Normal Resonance and Resonance Disorders
3. Can you define “resonance” and explain how it applies to speech?
I will define it this way. Resonance, as it applies to speech, is the quality of the “voice” (as distinct from pitch and intensity from phonation) that occurs when certain frequencies from the phonated sound are selectively enhanced based on the size and shape of the cavities of the vocal tract. This relates to the Source-Filter Theory, first proposed by Fant (1960), which says that sound is generated by vibration of the vocal folds (the source). The sound is then altered as it travels through the cavities of the vocal tract (filters) by the selective enhancement of formant frequencies. The selective enhancement of formant frequencies changes the quality (resonance) of the sound. It is actually resonance that gives us the uniqueness of our “voice.”
4. I know that both hypernasality and hyponasality are resonance disorders. What are the characteristics of each and how can I tell which one I am hearing?
Hypernasality occurs when too much sound enters the nasal cavity during production of oral speech sounds. This type of resonance makes the child sound as if he is “talking through his nose.” Hypernasality particularly affects vowels, which are resonance sounds. It can also cause oral plosives to be nasalized (substituted by the nasal sounds /m/, /n/ and /ŋ/). Hypernasality is usually caused by VPI, but can also be caused by a very large fistula following palate repair(Kummer, 2011a; Kummer, 2020a).
In contrast, hyponasality occurs when there is not enough sound entering the nasal cavity, specifically on nasal sounds, due to blockage in the pharynx or nasal cavity. This type of resonance makes the child sound "stopped up." Hyponasality can be caused by pharyngeal cavity blockage secondary to maxillary retrusion, adenoid hypertrophy, or even by tonsillar hypertrophy if the tonsils intrude into the pharyngeal cavity. Hyponasality can also be caused by nasal cavity blockage due to congestion, a deviated septum, polyps, or stenotic nares (Kummer, 2011a; Kummer, 2020a). The term denasality refers to a total blockage of the sound from entering the nasal cavity on nasal sounds. Because this is hard to determine, this term is rarely used.
5. What exactly is cul-de-sac resonance and what causes it?
Cul-de-sac resonance occurs when the sound energy enters a cavity of the vocal tract, but is blocked at the exit of cavity’s normal outlet. The sound is therefore trapped in a blind pouch. Because some of the sound is absorbed by the soft tissues, the speech/voice is perceived as muffled and low in volume. Like hyponasality, cul-de-sac resonance is due to obstruction, but in this case, the place of obstruction is at the cavity’s exit point rather than at the entrance or within the nasal cavity.
There are three types of cul-de-sac resonance, depending on the location of the blockage (Kummer, 2020a). All are defined by blockage at the cavity’s exit point. As such, oral cul-de-sac resonance occurs when the sound is partially blocked from exiting the oral cavity during speech. This can occur due to microstomia (a small mouth opening). It is also what is heard with “mumbling” or speaking without opening the mouth normally. To imitate oral cul-de-sac resonance, say oral sentences with a very small mouth opening. Nasal cul-de-sac resonance occurs when the sound is partially blocked from exiting the nasal cavity during speech. This is most noticeable when there is a combination of VPI (which would otherwise cause hypernasality), but also a blockage in the anterior part of the nose or nares. Nasal cul-de-sac resonance is commonly found in individuals with a history of cleft lip and palate, which can cause both VPI and either a deviated septum (due to a unilateral cleft lip) or a stenotic naris (due to scarring after a cleft lip repair). Nasal cul-de-sac resonance can be simulated by imitating hypernasality while closing one or both nostrils. Pharyngeal cul-de-sac resonance occurs when the sound is blocked from exiting the oropharynx during speech. This is typically caused by enlarged tonsils that block the oropharyngeal opening (exit of the pharynx). As with other types of cul-de-sac resonance, this blockage causes speech to be low in volume and muffled in quality. Although enlarged tonsils are the most common cause of pharyngeal cul-de-sac resonance, it can also occur due to scar tissue or other forms of obstruction on the pharyngeal wall of the hypopharynx or oropharynx. To imitate pharyngeal cul-de-sac resonance, produce oral sentences with your closed fist over your mouth.
Normal Airflow and Nasal Emission
6. How is airflow used with speech and why is it important?
Airflow from the lungs is needed to build up subglottic air pressure, which generates vocal fold vibration for phonation. Of course phonation is needed for all vowels and voiced consonants. Airflow is also important for oral articulation, particularly for the production of pressure-sensitive phonemes (e.g., plosives, fricatives, and affricates). Without the airflow, these sounds would be impossible to produce and would seem to be omitted in words and connected speech.
7. What causes nasal emission and when does it occur?
Audible nasal emission is caused by a leak in the velopharyngeal valve. It is heard during production of the pressure-sensitive phonemes, particularly voiceless phonemes, which don’t have the competing sound of phonation and also have more airflow than their voiced counterparts. A relatively small velopharyngeal opening actually results in more audibility of the nasal emission than a large opening because the air goes through the velopharyngeal valve and is released with more pressure. This causes bubbling of secretions, which is very audible. (This distortion has been called nasal turbulence or nasal rustle.) In contrast, a relatively large velopharyngeal opening causes more nasal emission, but in this case, the airflow is often inaudible because there is little resistance to the flow. However, the loss of airflow through the nasal cavity reduces or eliminates the needed airflow in the oral cavity for consonants. As a result, the pressure-sensitive sounds will become weak in intensity and pressure and may even seem to be totally omitted.
8. If there is not enough airflow for production or pressure-sensitive sounds, do children ever use compensatory strategies to increase intelligibility?
Yes, they do. If there is not enough airflow in the oral cavity to produce pressure-sensitive sounds, the child may compensate by producing these sounds in the pharynx, where there is airflow. Although placement is changed, the manner of production is typically maintained. Therefore, common compensatory productions for VPI include either glottal stops or pharyngeal plosives for stop/plosives and either a pharyngeal fricative or posterior nasal fricative for oral fricatives. It should be noted that compensatory productions are developed to increase intelligibility. Therefore, speech therapy to eliminate these productions (if successful) would actually decrease intelligibility unless the cause of the nasal emission (e.g., VPI) is corrected first.
Evaluation of Speech and Resonance
9. What speech samples do you use to evaluate resonance, nasal emission, and compensatory articulation productions?
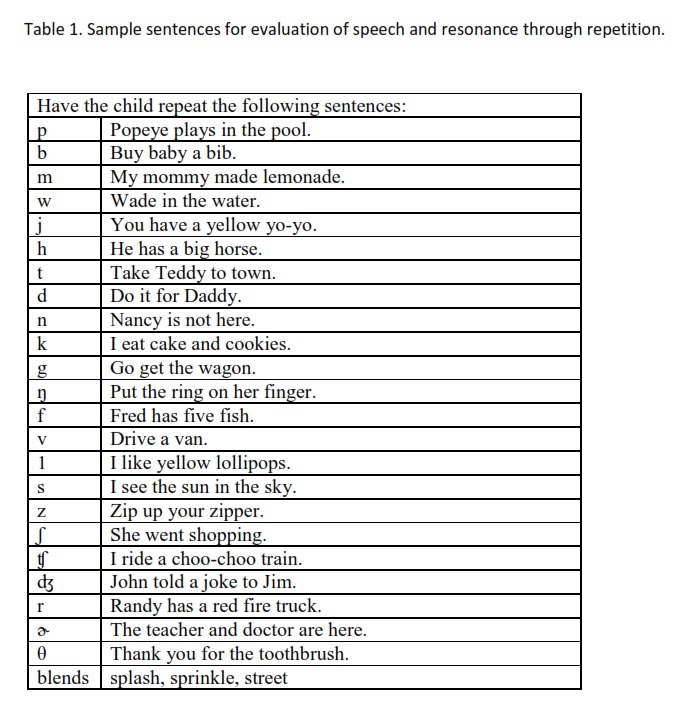
I am not a fan of single word articulation tests for several reasons. First, single words represent the child’s best production of the sound, not their typical production. In addition, these tests are time-consuming and expensive. Instead, I prefer to have the child repeat sentences that are loaded with sounds of the same placement. (See Table 1 for examples.) Additional sentences can be added as needed to further test errors. If the child is not able to repeat sentences, then I use a repetitive syllable test. In this test, I have the child do repetitions of syllables with each consonant followed by both a low vowel and then high vowel (i.e., /sɑ, sɑ, sɑ, sɑ, sɑ/ and /si, si, si, si, si/). These informal tests are faster, easier, cheaper, and actually more representative of the child’s typical production. In addition, these speech samples make it easy to test articulation production and resonance at the same time (Kummer, 2011c; Kummer, 2016; Kummer, 2020b).
10. How do I determine the type of resonance?
In your evaluation, first determine if resonance is normal with an appropriate balance of nasal resonance for nasal sounds and oral resonance for oral sounds (Kummer, 2011c; Kummer, 2016; Kummer, 2020b; Smith & Kuehn, 2007). If resonance seems abnormal, an easy way to distinguish hypernasality from hyponasality is to listen for the oral/nasal cognates. If oral voiced plosives sound more like their nasal cognates (e.g., m/b, n/d, ŋ/g), then the resonance is hypernasal. In contrast, if the nasal sounds seem more like their oral cognates (e.g., b/m, d/n, g/ŋ), then the resonance is hyponasal. If the voice is low in volume, consider hypernasality rather than hyponasality. If the voice sounds low in volume and also muffled, consider cul-de-sac resonance. Always do an intraoral evaluation which can give clues to the cause of abnormal resonance. Evidence of a repaired cleft or submucous cleft may cause VPI and contribute to hypernasality. In contrast, enlarged tonsils and evidence of mouth breathing suggest obstruction, which would contribute to either hyponasality or cul-de-sac resonance.
11. How do you determine the severity of hypernasality?
Rating severity is very difficult to do for several reasons. First, you would need ear training with many audio examples of different levels of severity. Then you would need a lot of practice. Despite this, it is difficult to achieve inter- and even intra-judge reliability. Ratings of severity are also complicated by the fact that the child with hypernasality is not that consistent. This is because the size of the velopharyngeal opening varies with the length and phonemic complexity of an utterance and also with the effort or fatigue. Therefore, resonance will be best in short utterances and with effort than in conversational speech, especially at the end of the day. The good news is that severity ratings do not impact treatment recommendations. The type of physical correction, including surgery, is based on the type of resonance (not the severity), the etiology, and in cases of VPI, the location of the opening. Therefore, the SLP’s job is to determine the type of resonance, which is not something that a surgeon can do.
12. What if I’m not sure about what I’m hearing? Are there any tools that can help me?
Certainly! My favorite tool is totally low-tech and very cheap. It is a straw! A straw will amplify sound that goes through it, just like a stethoscope, but it is less expensive and is disposable (Kummer, 2020b). (If you have concerns about the environment, you can also use any type of tube.) Put one end of a straw (preferably the short end of a bending straw) or tube in the child’s nostril and the other end near your ear. To determine if there is hypernasality, have the child produce syllables or sentences with only oral sounds. If you hear sound through the straw, then there is hypernasality. If you hear airflow, then there is nasal emission. Next, have the child produce syllables beginning with nasal sounds or a prolonged /m/. If there is no sound through the straw or the sound is muffled, then there is hyponasality. In this case, check both nostrils because there may be obstruction on one side and not the other.
13. Do you have any tips on how to do an intraoral examination and what to assess?
I’m glad you asked. The key to a successful intraoral examination is making sure that all oral structures are clearly visualized. If you ask the child to say /ɑ/ (as in “father”), you will not have a good view of the back of the oral cavity unless you push the back of the tongue down with a tongue blade. Instead, I recommend having the child say /æ/ (as in “bat”) instead (Kummer, 2020c). With this vowel, the back of the tongue goes down so that you rarely need to use a tongue blade. In addition, you can ask the child to try to touch his tongue to his chin, which will bring the tongue forward as well. This opens up the entire oral cavity, including the back.
To visualize the surface of the hard palate or velum, a dental mirror is especially helpful. The mirror should be placed under the palate. The light from a flashlight should then be directed on to the mirror. In this way, the light will be reflected off the mirror and will illuminate the surface of the palate above it. This is particularly useful when examining the hard palate for a fistula (Kummer, 2020c).
Now that we have talked about methodology, let’s talk about what observations are important to make. Perhaps the most important observation for speech sound disorders is the relationship of the tongue tip to the alveolar ridge. If the tongue tip is anterior to the alveolar ridge (as with an anterior crossbite or Class III malocclusion) or if the tongue tip is posterior to the alveolar ridge (as with Class II malocclusion), this will cause obligatory distortions of speech. If the teeth interfere with tongue tip movement or anterior movement of the airstream, this will also cause obligatory distortions. Because obligatory distortions are due to abnormal structure (as opposed to abnormal function), they cannot be corrected with speech therapy. Instead, correction of the structure is needed.
Important observations that could be related to hypernasality include evidence of a submucous cleft, a relatively short velum, or an oronasal fistula. Important observations that could be related to hyponasality include enlarged tonsils or an open mouth posture with anterior tongue position. Finally, important observations that could be related to cul-de-sac resonance include a small mouth opening, enlarged tonsils, or stenotic nares.
14. Can you guide me as to where I should refer a child once I determine that there is a resonance disorder?
Absolutely. Most SLPs automatically refer the child with suspected structural disorders to an ear, nose and throat specialist (ENT). This is totally appropriate for children who exhibit signs of obstruction, causing either hyponasality or cul-de-sac resonance. This is NOT appropriate for children with hypernasality and/or nasal emission due to VPI. The reason is that evaluation and treatment of VPI is a specialty area. General ENTS are not trained in this area. Therefore, it is important to refer a child with evidence of VPI to a cleft/craniofacial center where there are specialists (SLPs, ENTs and surgeons) who will be able to confirm the diagnosis and treat the child, as appropriate.
Treatment
15. Can hypernasality be corrected with speech therapy?
Hypernasality due to VPI cannot be corrected by speech therapy. Instead, VPI requires physical management, which means surgery, or a prosthetic device if surgery is not an option (Kummer, 2011d; Kummer, 2020d).
16. Can nasal emission be corrected with speech therapy?
As with hypernasality, nasal emission cannot be corrected with speech therapy if it is caused by VPI. Speech therapy is only appropriate if the nasal emission is phoneme-specific, in that it only occurs on certain sounds (e.g., /s/ or other sibilants) and it never occurs on plosives. Phoneme-specific nasal emission is caused by the substitution of either a pharyngeal fricative or posterior nasal fricative for one or more of the sibilant sounds. This causes the airstream to be emitted through the nasal cavity. By changing placement from the pharynx to the oral cavity, the nasal emission will disappear. Phoneme-specific nasal emission can be due to a compensatory production that persists after surgical correction of VPI. It can also occur as a misarticulation (due to mislearning) in a child with no history of VPI (Kummer, 2020d).
17. Can compensatory articulation productions be corrected with speech therapy?
The answer is clearly a YES… and a NO. It is very difficult, if not impossible, to correct placement of a compensatory production while there is still VPI. If you could correct the placement, it would actually decrease intelligibility. Therefore, it is best to wait until after surgical correction to correct these productions. Therapy will be much faster and more successful at that time. (See “Speech Therapy Cookbook” for specific articulation placement strategies in Cleft Palate and Craniofacial Conditions: A Clinical Guide to Comprehensive Management [Kummer, 2020d]).
18. My colleagues often use oral-motor exercises for children with resonance problems. Do you recommend that?
I NEVER recommend oral-motor exercises for the following reasons, that can be found in the literature (Lof, 2008; Lof, 2011; Ruscello, 2008a; Ruscello, 2008b:
- There is absolutely no evidence that nonspeech exercises work for speech sound disorders or for VPI.
- There is no logical reason to use exercises. “Exercises” are designed to strengthen muscles or restore muscles to baseline. Velopharyngeal insufficiency is caused by a structural abnormality, not a muscle weakness problem, so exercises don’t make sense. Velopharyngeal incompetence is due to a neurological cause, but exercises don’t work for this disorder either.
- Even if muscle strengthening worked, the child would have to do the muscle exercises the rest of his life to maintain the added strength.
- Hyponasality and cul-de-sac resonance are both due to obstruction in the vocal tract. Exercises won’t eliminate obstruction.
In almost all cases, resonance disorders require physical management, not exercises or even speech therapy.
19. Once VPI is surgically corrected, does the child need intensive speech therapy postoperatively?
I never recommend intensive speech therapy. Instead, I recommend weekly therapy with intensive practice at home. Here's the thing... The purpose of speech therapy is to teach the child a skill, such as how to produce a certain speech sound. As consistent with motor learning principles (Maas, Austermann Hula, Freedman, Wulf, & Ballard, 2008), we give the child instructions, the child goes through a period of trial and error, and then we give feedback. The motor learning part of the therapeutic process involves "skilled work" and is what we do in speech therapy.
Once the child is able to produce the sound, it is then important to work on motor memory. Motor memory is what helps the child be able to produce the sound automatically, without conscious thought, so that there is “carryover” into connected speech (Maas et al., 2008). The key to achieving motor memory practice! The practice part of the therapeutic process is not always "skilled work" (which is a requirement for healthcare reimbursement) and therefore, should primarily be done at home. I always say to parents: “Speech therapy is like taking piano lessons. If you just go for the lesson and don't practice at home, you won't learn to play the piano.” The same principle applies to other motor learning activities, including learning to play a sport.
Because practice at home is critical to therapeutic success, it is important to train the parents on how to work with the child at home. The parents should be instructed to practice with the child every day and several times a day, because frequent, distributed practice has been shown to result in the most rapid progress. That sounds like a lot. However, 30 seconds can be considered a practice session.
Finally, it is important to consider the “dose” that the child receives in every therapy or practice session. In this case, I will define dose as the number of correct productions achieved. We can’t predict the dose that will be needed for a particular child to start using a newly acquired speech sound automatically in connected speech. However, we do know that the higher the dose in sessions, the faster the progress will be. Therefore, drill work is important, which is consistent with motor memory principles.
20. Do you have any last thoughts?
Yes. In my career, I have seen so many children with VPI, or even dental anomalies, who are receiving speech therapy, when the problem is abnormal structure—not abnormal function. Of course, these children do not make any progress, and therefore, are continually discouraged. This is a waste of time and money, but most of all, unfair to these children and families. It is our responsibility as speech-language pathologists to make a differential diagnosis between distortions that are due to abnormal function versus those due to abnormal structure so that the child receives appropriate services.

