Communication Access Real-time Translation (CART) is provided in order to facilitate communication accessibility and may not be a totally verbatim record of the proceedings. Consumer should check with the moderator for any clarification of material.
This article is a written transcript of the course, “The Dysphagia Workout: Applying Exercise Principles into Treatment”, presented by Lori Burkhead Morgan, Ph.D., CCC-SLP on September 21, 2011.
>> Amy Natho: Hello, everybody, I welcome you to the SpeechPathology.com virtual conference on Dysphagia Management. We're very excited that you could join us today, and hopefully throughout the week as well, to hear the latest on Dysphagia Management from a really outstanding group of presenters. Today's expert seminar is titled “The Dysphagia Workout: Applying Exercise Principles into Treatment” and it is presented by Lori Burkhead Morgan. My name is Amy Natho and I will be your moderator today.
At this time I'm very honored to introduce Dr. Lori Burkhead Morgan. Dr. Burkhead Morgan has practiced speech-language pathology since 1994 in a variety of settings. She earned a Ph.D. from the University of Florida in 2005, focusing on using exercise-based principles in dysphagia diagnosis and management. She has presented domestically and internationally, published a peer-reviewed article and a book chapter relating to dysphagia. Her current research focuses on developing more effective approaches for dysphagia evaluation and treatment. So welcome, Lori. Thank you so much for joining us today.
(applause)
>> Lori: Thank you so much, Amy. I’m so excited to be here. I see that there are over 131 participants, and I am just thrilled and flattered that you all decided to log-in and participate in my course today. I hope to give you some very usable, functional information on exercise principles and also how to apply the practice. So at the end of today's discussion you should hopefully have some information that you can implement immediately into your clinical treatment sessions.
Purpose of this Talk
- I would like to begin our discussion with muscle structure and function. I will have a couple of technical slides to start out with, but I think it is important that we all have an understanding of muscle structure, how it forms and how it works and how it can get stronger and weaker as well.
- I'm going to talk to you about the muscles’ response to both conditioning as well as deconditioning.
- Then, I will talk to you about some exercise applications and evidence-based practices in the dysphagia rehabilitation field.
Neuromuscular Development
To begin with, I would like to talk to you about neuromuscular development. As our bodies are developing, there are certain proteins during embryotic development that are present. These proteins are there to predetermine which tissue becomes muscle. There are cells called myoblasts that form and get linked up with motor nerves. Together, these form the neuromuscular junction.
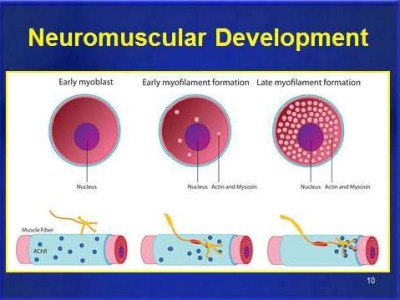
Muscles are initially covered with acetylcholine receptors which are represented here by the tiny blue dots. Those acetylcholine receptors concentrate to where the nerve endplate attaches itself on the cell. As you can see, they basically move and concentrate right there at that motor endplate. In adult denervation (as in disease or injury) the process actually happens in the reverse. The acetylcholine receptors concentrated at the endplate begin to spread out of the muscle fiber as injury or disease occur. What's great to know is that this system is very highly plastic from cradle to grave, so as it develops and degenerates and acetylcholine receptors move away from the endplate, they can also come back to the endplate. As we stimulate patients and get them exercising, this system reorganizes back to its original intent. That's great news for us.
How Muscles Work
Next I just wanted to talk with you about how muscles work.
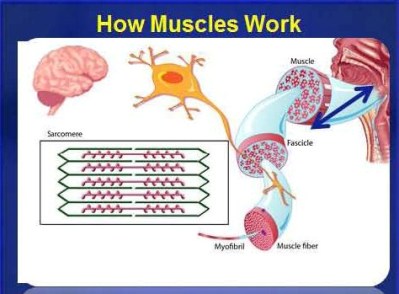
As you can see here in the picture, the muscle forms in a hierarchical pattern. It is a very specialized way that these muscles form to create movement. Muscle cells actually are very small cylindrical fibers that are smaller than human hair. These fibers are broken down into functional units. The largest functional unit, as you see on the bottom of this picture, is the myofibril. The myofibril is arranged in parallel, and thousands of these together form muscle fibers. That adds to the diameter and the bulk of muscle and that's where we get the concept of strength. The greater the diameter, the greater force-generating capacity of the muscle, and we all sort of know that. Someone who has big beefy muscles, you know they're probably pretty strong and that's because they have a lot of myofibrils in parallel with each other.
Myofibrils are further subdivided into little units called sarcomeres, and these units are arranged end to end. This is what we consider to be the workhorse of contraction. Now, the number of these cells is determined by the length of a muscle as opposed to the girth of a muscle, and they’re broken down into filaments with proteins called actin and myosin. The actin and myosin on your diagram are represented by the pink little numbers sticking off of these long lines. Those are what really make the muscle contract. These contain the proteins actin and myosin. Myosin generates tension in the muscle and actin helps regulate that, so there isn't too much spasticity. Tropomyosin is another protein that regulates and turns on the contraction cascade within the muscle. So if we put all of this together, there's a signal that comes from the central nervous system and then that travels down the axon. That action potential arrives at the neuromuscular junction. At that point acetylcholine is released and that causes the muscle fiber excitation deep into the fiber. A chemical reaction begins causing the actin and myosin to interact and cycle both contraction and relaxation, pulling that muscle tight and shortening it. So as the shortening occurs, that's what we consider contraction.