Editor’s note: This text-based course is a transcript of the webinar, Dementia Diaries Part 1: Understanding the Types of Dementia, presented by Amber B. Heape, ClinScD, CCC-SLP, CDP, CMDC.
Learning Outcomes
As a result of this course, participants will be able to:
- List the types of dementia and their salient characteristics; eg, reversible or irreversible.
- Describe definitive diagnosis symptoms and neurological hallmarks of various types of dementia.
- Identify risk factors for cognitive decline in patients in order to improve clinical judgment about the necessity of evaluation.
Introduction
This is the first part of a four-part series discussing the types of dementia. In this series, we are going to be looking at dementia symptoms that affect a population that we are dedicated to serving. I hope this course series rejuvenates you as a practitioner or helps you remember why you chose this profession. I do not claim to know everything, nor do I believe any of us ever will. However, we all should be lifelong learners.
The Aging Population
According to data from 2018, there are over 51 million people at social security age or older living in this country (2018 Profile of Older Americans. Retrieved from www.aca.gov). This population is a third bigger than it was a decade ago. In this country, approximately one in every seven people are considered elders. However, with that increase in age also comes an increase in the potential for chronic health conditions. Medical science is helping us live longer, and as we live and age, we may have some type of chronic health condition.
Aging and Dementia
The Alzheimer’s Association’s 2019 report states that in the United States:
- 5.8 million people are currently living with Alzheimer’s Dementia (AD)
- One in ten people over age 65 has Alzheimer’s
- This number increases to one in three over the age of 85
- Almost 2/3 of those with AD are women
- The lifetime risk of a person for developing AD by age 65 is as high as 12% of men, but 21% of women!
(2019 Alzheimer’s Disease Facts and Figures. Retrieved from www.alz.org)
Some of last year’s information was published by the Alzheimer's Association specifically on Alzheimer's disease. There are approximately six million people currently living in the United States with Alzheimer's disease and dementia. This means that one in 10 people fall in that elderly population. As we grow older than 85, that increases to about one in three people. My mom will turn 65 this year and my grandmother is in the 85 and older category. Many of you most likely have friends and family members who fall into this category as well.
If you are like me, you are constantly looking for signs and symptoms. We know that there is a decent risk of a person developing Alzheimer's dementia, especially as a woman. There appears to be some hereditary link as well. In my family, almost all of my grandparents and great-grandparents had Alzheimer's disease at some point in their life.
Aging and Dementia - Demographics
When we look at the demographics of dementia, there is a major disparity. When we look at minority groups, African Americans and Hispanic Americans, we find that minority groups are much more likely to have Alzheimer's dementia than European American groups. If you are African American, your risk is twice as high. If you are Latino or Hispanic, your risk is anywhere from about 1.25 to 1.5 more times likely.
The highest percentage of increases in dementia are projected to occur over the next five years in 5 states:
- Arizona: 43%
- Nevada: 36%
- South Carolina: 30%
- Vermont: 31%
- Wyoming: 30%
Arizona is projected to have a 43% increase. I live in South Carolina so a 30% increase is rather alarming to me. We have this large number now but it is going to be even higher in the next five years. I truly believe this is where we, as speech-language pathologists, are going to be essential as health care providers. We are going to be fighting the characteristics and the symptoms that are coming along with some of these increased diagnoses of dementia, whether that is with aphasia and word-finding or whether that is an increase in dysphagia.
Dementia - “The Ticking Time Bomb”
If you have ever read anything by Dr. Peter Piot, he calls dementia the "ticking time bomb." I know right now with what is going on in this country, it already feels like a ticking time bomb. However, when we look at dementia, the World Health Organization reports that every four seconds a new case of dementia occurs. I have been talking for almost eight minutes already. Think about how many new cases of dementia have occurred during those eight minutes. It is the number one cause of disability requiring long-term care due to the dependency among older adults. And because we have had an increase in our knowledge of dementia, about 95% of the general public believes that dementia could affect them at some point in their life. Another alarming statistic is that 35% of caregivers have concealed their loved ones' diagnosis. Whether that is because they are in denial themselves or whether that is because they are trying to protect their loved one, could be up for interpretation. The annual cost worldwide is about one trillion dollars, and it is not a part of normal aging despite what the majority of healthcare practitioners may believe (World Alzheimer Report 2019, World Health Organization).
Dementia (Major Neurocognitive Disorder)
The Diagnostic and Statistical Manual of Mental Disorders, DSM-5, is now in its fifth edition. It now calls dementia a major neurocognitive disorder. They use that terminology, but the word dementia continues to be an acceptable term as well. It is important to note that dementia in itself is not a disease. Oftentimes, it is caused by a specific disease perhaps one of which we will discuss today.
When you have dementia, most people have memory loss as their primary symptom that indicates something is wrong. The DSM-5 considers dementia to be a group of symptoms that are characterized by a loss of function like attention, executive function, memory, learning, language, perceptual-motor function as well as social cognition.
Dementia-Primary Categories
Let's move onto the types of dementia. There are a couple of primary categories that I want to discuss. The major two are reversible and non-reversible, and then under that non-reversible umbrella, we have progressive and non-progressive. We are going to break all of those down and talk about some of the different causes of each of these types of dementia.
Reversible Dementia
- D - drug reaction, overdose, toxicity, anesthesia
- E - emotional disorders (depression)
- M - metabolic or endocrine (thyroid) issues
- E - eyes and ears (sensory loss)
- N - nutritional deficits
- T - tumors
- I - infection (sepsis, UTI, pneumonia)
- A - arteriosclerosis
First, are reversible dementias. Some medical doctors will claim that reversible dementias are not dementias, or that they are delirium. The National Council of Certified Dementia Practitioners classifies them as dementias, and because I am a CDP, I also classify as reversible dementia, but we are going to discuss a little bit of that as we go.
In reversible dementias, the onset is abrupt. The decline is acute right after some type of incident typically. We are seeing quite a bit of this right now. In fact, we are seeing some signs of delirium or reversible dementia due to the social isolation that is occurring because of COVID-19, whether that is social isolation in a long-term care facility, an assisted living facility, or out in the community and in homes. People who normally would have a lot of social interaction are now having to practice social distancing. People are not able to just go out and go to the grocery store as they were before. My mom lives across the street, and we check on her all the time, but I refuse to allow her to go to the grocery store. I am very adamant that she still does cognitively stimulating tasks during this time because I do not want to see the decline in cognition.
When we look at reversible dementias, it is important to note that we do what we can to take away the cause of reversible dementias and then we assess to see if spontaneous recovery has occurred. If spontaneous recovery does not occur, then that is when we intervene with treatment. We need to take away the cause before we try to treat because if the cause is still present, then our etiology is there and we are not going to be able to do as much to change those symptoms.
The research shows though that after that period of spontaneous recovery, adults may be left with long-term deficits without our intervention. I believe that this is where our profession, in the next year or two or maybe even over the next six months, is going to see a boom in patients. The social isolation will be taken away, but these patients may not spontaneously recover as they should. They will need our intervention in order to try to get back to that prior level of function.
I have seen some different research about what typical spontaneous recovery periods are after anesthesia especially on knees and hips that have been replaced. Research says three hours post-op is a typical recovery. I have seen other reports that it is more like a couple of days. Regardless, if you are working in post-acute rehab or in skilled nursing, by the time those patients get to you they should be passed that spontaneous recovery time frame. Thus, if you are doing the Brief Interview of Mental Status (BIMS) to assess for their cognition, under the new PDPM payment model, and you see their BIMS score shows that they have a cognitive deficit, then we cannot expect them to jump right back in and be normal again without our intervention. Again, this is because the typical spontaneous recovery time has passed.
Emotional disorders and depression are a huge cause of reversible dementias. Hence, the social isolation components that are occurring here in 2020 are going to affect many clients down the road. Thyroid issues, sensory loss, nutritional deficits, tumors, and coronary artery disease are other areas that contribute.
Anytime you see a patient who has had any type of cardiopulmonary condition, with reduced blood flow or oxygen, this may be the only etiology that we see, but these patients are showing symptoms of dementia. If you have worked in healthcare for any length of time, you have definitely seen this with UTI, pneumonia, sepsis, gangrene, or any type of infection in the elderly population. You will see their cognition tank. What we know is that once those antibiotics are given and that infection is gone, we should see spontaneous recovery, and if we do not, then this is when we intervene.
Below is some of the information that I just discussed. These studies are listed in your references as well.
- Infection (UTI, Sepsis, Pneumonia, Gangrene…)
- The American Academy of Neurology recognizes that new or past infections can contribute to cognitive impairment
- NIH study documented sepsis was associated with later cognitive and physical decline
- Journal of AMA says that adults with infection “may be left with moderate/severe cognitive deficits and functional disabilities”
- Anesthesia
- British Journal of Anesthesia:
- Increased evidence that major neurological changes can occur post-anesthesia
- Brain particularly vulnerable at the beginning or end of life
- The earliest manifestation of neuronal damage is a decrease in higher cortical functions of storage and recall of memory and cognitive processing
- British Journal of Anesthesia:
- International Anesthesia Research Society
- Recognizes POCD- Post Operative Cognitive Dysfunction
- A study found that 10-15% of the elderly have postoperative cognitive decline at 3 months post-op
- Surgery may “unmask” intellectual declines already present
- Cognitive decline may result from inflammatory processes after anesthesia
- Recognizes POCD- Post Operative Cognitive Dysfunction
- Research on Anesthesia vs. Analgesic effects:
- A study on knee and hip replacements with different types of anesthesia and cognitive function suggested that normal cognitive recovery from both types happens within 6 hours post-op
I have encountered a lot of people in healthcare over the past 16 years that are very adverse to cognitive-linguistic, cognitive-communication therapy. What I say to them is that when you look at the research and if you go on the ASHA Practice Portal, the evidence shows that these etiologies, infections, anesthesia, et cetera absolutely cause dementia. Another thing about post-operative cognitive dysfunction is that many times patients who may have been able to mask their deficits before their operation, suddenly are unable to do so. You may have to ask a lot more probing questions of the patient and/or their family members in order to really determine if there were deficits before the procedure.
What Else Can Contribute to Decline?
Prolonged hospitalization is another cause of decline, and this is where that dementia delirium overlap or coexistence often happens. When you look at patients who have extended hospital stays or extended ICU stays, you often will see what physicians refer to as delirium. However, once they are out of that environment and it does not spontaneously resolve, we have to see if it is dementia versus delirium.
The Mayo Clinic, a very reputable institution, produced a publication that referenced the strongest risk factors for mild cognitive impairment or mild neurocognitive disorder (see below). When you look at this list and you think of your parents, grandparents, patients, and maybe even yourself, many fall into quite a few of these categories. As we will discuss in a later session, we need to do our best to mitigate the likelihood that that may occur.
- Increased Age
- APOE- e4 gene
- Diabetes
- Smoking
- Depression
- Hypertension
- Hypercholesterolemia
- Lack of physical exercise
- Infrequent participation in mentally or socially stimulating activities
Non-Reversible
Non-Progressive Dementias. Non-reversible, non-progressive dementias are typically from an abrupt onset like a traumatic brain injury, an anoxic incidence, or respiratory failure. A single CVA can also contribute to that. We are going to talk about more of a progressive type of dementia related to CVA a little later, but when you look at a single CVA, this would typically be considered a non-reversible, non-progressive type of dementia.
Progressive Dementias. I also want to talk about many of these non-reversible progressive dementias listed below, but there are others that I have not put on this list such as progressive supranuclear palsy, corticobasal syndrome, and dementia due to muscular sclerosis. There are some common types and some less common types, and then there are some rare types of progressive dementias.
- Chronic Traumatic Encephalopathy
- Parkinsons
- Multi-Infarct
- Fronto-temporal
- Lewy Body
- Huntington’s Disease
- Creuxfeldt-Jakob
- Korsakoff Syndrome
- Normal Pressure Hydrocephalus
- HIV Infection
- Alzheimer’s Disease
Progressive dementias have a gradual onset. They are progressive as the name implies, but they could be slow, or if other factors are present or some of those acute incidents occur while this progressive dementia exists, you could see a very quick progression. For example, you may have a patient with Alzheimer's disease. If this patient falls and breaks a hip and goes into the hospital, the patient's cognitive score may go from a GDS3 to a GDS5. We will discuss those GDS levels next time. This is a major decline. This is the difference between being able to live on your own to requiring long-term care. This happened to my own grandmother. Anesthesia and hospitalization really took a toll on her Alzheimer's disease, and she had a very rapid decline. I have seen this happen a lot. A client with some baseline deficits but is otherwise pretty stable can rapidly decline with something as simple as a hip replacement.
Chronic Traumatic Encephalopathy (CTE)
The first type of dementia I want to discuss is CTE. If you have seen the movie "Concussion" with Will Smith, you will know exactly what I am talking about. It's chronic traumatic encephalopathy. It is also called dementia pugilistica or in boxers, "punch drunk." This is dementia that is common in people who have had repeated concussions or repeated head injuries. With those repeated head injuries, there is increased tau protein in the brain and neurofibrillary tangles occur. This contributes to a rapid decline that you may see.
There is a lot of national media attention on CTE, and I recently had a very close friend whose father passed away that played football in high school, college, and semi-pro. He was also a football coach for 30 years. She was just talking about all of his symptoms and alarm bells started going off in my head. I told her to talk to his doctor to see if it could be CTE. She looked up the characteristics on the internet, and she said that he had every single symptom that was listed. He ended up passing away before they got a definitive diagnosis, but we are seeing a very delayed diagnosis of about eight to ten years after a football career or after serving in the military in combat.
Symptoms. After those traumas, we are seeing patients coming in with headaches and loss of attention/concentration. We are seeing patients with very short tempers who blow up. There are also gait and speech abnormalities, behavioral issues including depression and suicidal thoughts, and even some tremors that almost look Parkinsonian. When doing a case history, it may be a good thing to ask if they have had repeated head injuries or repeated concussions in their life. Did they play sports like hockey, football, boxing, et cetera?
Parkinson’s Disease-Related Dementia
Anywhere between 50 and 80% of people with Parkinson's disease will actually experience dementia. Typically, it takes about 10 years from that diagnosis at onset until that dementia really starts to rear its ugly head. One of the major triggers is stress. When we look neurologically at Parkinson's dementia, we see beta-amyloid plaques and tangles, but typically with Parkinson's dementia, you will see motor symptoms first. We are going to talk about Lewy body dementia in a few minutes, and motor symptoms for that diagnosis show up later, but for Parkinson's disease, motor symptoms occur first and then you will see the cognitive symptoms down the line. Treatment may include medications as well. (Alzheimer’s Association, 2016)
Symptoms. When you see a patient that has Parkinson's disease-related dementia, you may see a shuffling gait, a stooped posture, and a forward head. Many times you will see symptoms more unilateral than bilateral. They will also have tremors, akinesia, abnormal movement patterns, and sometimes a very emotionally labile facial expression that is mask-like.
Multi-Infarct (Vascular) Dementia
The next type of dementia is vascular dementia. This is the second most common type of dementia behind Alzheimer's disease, but it is important to note that multi-infarct or vascular dementia (those terms are interchangeable) and Alzheimer's can coexist. When they co-exist, you are typically going to see a more severe case. Vascular dementia is more common in men aged 55 to 75. This is because CVAs are more common in men than they are in women.
I live in a county in rural South Carolina that has the highest per capita endstage renal disease, diabetes, and stroke rates in the entire state. It is a very high-poverty, Title 1 county. I chose to move back here because this is where I grew up, and I wanted to come back into this rural community and give back. The stroke rates in this community are very high, thus the incidence of multi-infarct dementia is also a lot higher in my county. Multi-infarct dementia can occur from TIAs or multiple TIAs, as well as CVAs. I have had people tell me that they have never had a stroke, but they have had many TIAs.
Risk factors include:
- Diabetes
- Atherosclerosis (hardening of the arteries)
- Hypertension
- Smoking
- Alcohol abuse
- Stroke
- Poor diet/exercise
- Poverty may be a risk factor
It is very difficult to distinguish Alzheimer's dementia from multi-infarct dementia without a thorough case history as well as imagery because the symptoms are very similar.
Symptoms. Symptoms can include:
- Difficulty with tasks that used to come naturally or easily
- Becoming lost on familiar routes
- Word finding difficulties
- Losing interest in prior hobbies
- Flat affect/mood
- Misplacing items more often
- Personality changes
- Loss of social skills
- Change in sleep patterns
- Difficulty with basic tasks
- Safety awareness deficits
- Agitation
- Depression
- Short-term memory loss
When we look at the symptoms of multi-infarct or vascular dementia, you will hear about people who have been going to the grocery store their whole life, and suddenly, they become lost on their way. You may see word-finding difficulties. People who are avid newspaper crossword completers refuse to do it anymore. They become more aware of their deficits and may get frustrated and agitated as these tasks become harder.
Fronto-Temporal Dementia (Pick’s disease)
The next type is Pick's disease also known as frontotemporal dementia. In Pick's disease, the hallmark sign is a major change in personality. The frontal and temporal lobes of the brain are typically affected. There is nerve loss and there is a shrinking of the brain. We will look at some Alzheimer's images in just a little while, but Pick's disease looks similar in the way the brain appears to have shrunk.
When you look at all the different types of dementia, you'll see an onset to death progression from anywhere from six months to 20 years depending on the type of disease that causes dementia and the progression of it. Pick's disease is genetic. Patients with the Pick's are typically younger than your other patients. While patients can learn to compensate for the deficits using some of those remaining skills, pharmacologically there is nothing that has been shown to slow the progression of the disease. We can treat the behavioral issues but the disease itself will progress.
Symptoms. Here are some of the symptoms that we may see in frontotemporal dementia:
- Marked changes in personality and mood
- Communication and motor disruption highly prevalent
- Impaired judgment, impulsivity
- Boredom, apathy
- Inappropriate social behaviors
- The patient often unaware of the decline in function or inappropriateness
- Difficulty with language (receptive and expressive)
- Memory remains largely intact
Your patient may be sexually inappropriate. They may have a great memory but on pragmatic abilities, they are not so great. And, they are often unaware that it is inappropriate. They are not embarrassed by it because they are not even aware it is there. They often have fluent or nonfluent aphasia. You may also see a change in personal hygiene.
Lewy Body Dementia
Lewy body dementia on imaging looks a lot like Parkinson's disease dementia. It is largely under-diagnosed. You will see cognitive deficits first and physical deficits later. The average survival is only about five to seven years with Lewy body, and they will differentiate between Parkinson's and Lewy body by dopamine transporter PET scans.
Symptoms. Symptoms of Lewy body are very similar to the ones that I just listed with Parkinson's disease. The big difference is in Parkinson's there are unilateral symptoms, whereas, with Lewy body dementia you often see bilateral symptoms.
- Emotionally/physically labile
- Hallucinations (recurrent, detailed)
- Confusion varies widely from one day to the next
- Shuffling gait and stooped posture
- Depression
- Motor symptoms usually bilateral
- Cognitive impairments begin either before or within 1 year of motor symptom onset
- Repeated falls
- Unexplained loss of consciousness
- Visuospatial abnormalities
Huntington’s Disease
Next is Huntington's disease. You will hear it called Huntington's chorea sometimes. It is a genetic condition and typically affects very young people in the 30 to 40 age range. There have been cases of children as young as two years old with Huntington's disease and related dementia. There is really no known cure or way to slow the process.
Symptoms. Below are some of the things that you will see in Huntington's disease. The fidgety movements are very hallmark, and then the obsessive-compulsive behaviors and hallucinations are also two very common symptoms.
- Confusion
- Diminished coordination
- Fidgety, uncontrolled movements (upper body)
- Behavior changes
- Mood changes
- Anger and irritability
- Memory loss
- Hallucinations
- Decreased reasoning skills
- Obsessive-compulsive behaviors
Creuxfeldt-Jakob Disease (CJD)
There are two types of CJD - classic and variant. Variant CJD is more commonly known as mad cow disease. If you have been around any length of time, you would definitely remember when the mad cow disease outbreak happened.
In that mad cow disease outbreak, many cows and calves had to be slaughtered because of the outbreak of CJD. It is an infectious form of dementia and 90% of the patients who get CJD die within one year. Luckily, there are not very many cases that occur. It is rare, but when it does occur, prion protein attacks the healthy cells and changes them into abnormal shapes and destroys them rapidly (Alzheimer’s Association, 2016).
Symptoms. Some of the symptoms of CJD, mad cow disease, that you will see are listed below. These are things you would probably expect when you think of your cells being destroyed including things like blindness, severe dysphagia, and seizures. This has a rapid onset with no known cure.
- motor symptoms (ataxia, muscle twitches)
- confusion
- agitation
- memory loss
- severe dysphagia
- personality changes
- seizures
- sleepiness
- dysarthria
- blindness
Korsakoff’s Syndrome
Our next syndrome is Korsakoff's syndrome. If you have a patient who has chronic alcoholism, you may see Korsakoff's syndrome. A therapist called me about two weeks ago talking about a patient, and I asked if the patient had Wernicke's encephalopathy. She said that she was not sure, but she thought he had Wernicke's aphasia and receptively he was very slow. He had a history of alcohol abuse. Again, the light bulb started going off, and I thought of Korsakoff's syndrome. One in eight people who have chronic alcoholism will develop Korsakoff's syndrome.
Symptoms. This is one of the saddest types of dementia to me personally. I have seen brilliant PhD level professors who suffered from Korsakoff's syndrome. They have staggering, stumbling, confabulation, and tell crazy stories that never happened. They have a lot of jerky movements and stumbling and socially inappropriate behaviors. Wernicke's encephalopathy is a precursor to Korsakoff's syndrome or Korsakoff's dementia.
- Motor deficits (staggering, stumbling)
- Confabulation (making up information but believing it, often very detailed)
- Disorientation
- Memory loss
- Impaired reasoning skills
- Malnutrition
- Jerky eye movements
- Major changes in personality
- Lack of insight into the current condition
- Socially inappropriate behaviors
Normal Pressure Hydrocephalus (NPH)
Normal pressure hydrocephalus occurs when you have a subdural or subarachnoid hemorrhage, head trauma, a neurological infection, surgical complications, or a tumor. My mother-in-law has NPH from an aneurysm, and she has a permanent shunt. Without that shunt, her cerebrospinal fluid would put pressure on her brain. We saw the NPH dementia going on with her until she got that shunt. Typically, with many patients, once you have that excess CSF drained off, some of the symptoms go away but it may not. It may be a long-term process.
Symptoms. With NPH, you may see patients who get stuck or freeze in their movements. My mother-in-law would suddenly just stop when walking. You may also see a loss of continence. If you do not place a shunt and get some of that pressure off the brain, those symptoms will worsen to the point where it will cause permanent neurological damage. You often see lots of falls, issues with balance, et cetera. NPH is something that can be treated and managed when it is caught early.
- Difficulty walking (getting stuck or “freezing”)
- Slowing of movements
- Decreased executive functioning
- Loss of continence
- Symptoms will worsen over time if the condition remains untreated
- Apathy and withdrawal/ changes in mood
- Memory loss
- Sudden falls
HIV-Associated Dementia
Fortunately, there are many treatments available now that focus on those T-cells and reducing the viral load of HIV in patients. However, early in the disease process, the HIV virus will cross that blood-brain barrier and act as a Trojan horse to the brain causing inflammation that can result in encephalopathy.
Symptoms. You will see patients who become very apathetic, depressed, and socially withdrawn. They either sleep all the time or they never sleep, and they have manic and psychotic type episodes. You might also see dysarthria in speech with HIV-related dementia.
- Memory loss
- Mental fog
- Dysarthria
- Apathetic response to activities previously enjoyed
- Reduced coordination
- Decreased motor skills
- Changes in personality and behavior
- Depression
- Social withdrawal
- Sleep disturbance
- Psychosis/mania
- Seizures
Alzheimer’s Disease
Everyone has heard about this type of dementia. It is the most commonly diagnosed type, but as many people including healthcare practitioners believe, it is not a normal part of aging. You should not significantly lose your memory and your language function just because you are aging. Typically, Alzheimer's disease is diagnosed in the mid-60s. A hallmark of Alzheimer's is memory loss, especially short-term memory - patients who can remember what they did 20 years ago but not what they did 20 minutes ago.
It used to be that Alzheimer's disease could only be diagnosed on autopsy for a definitive diagnosis, but now we can have pre-mortem diagnoses occurring. There are beta-amyloid plaques and tangles in that brain structure, and you will almost see a wasting of the brain. I describe it to patients as a shrinkage of the brain. There is a major genetic link. I know my risk is extremely high because of genetics, but I am very hopeful about the current research on slowing or preventing Alzheimer's.
Symptoms. There are different stages: mild, moderate, and severe. The symptoms differ by stages:
- Mild - memory loss, safety issues, difficulty paying bills, executive functioning skill loss
- Moderate - increased confusion, significant language deficits, behavioral issues begin
- Severe - unable to communicate verbally, completely dependent on caregivers, dysphagia prevalent
Beta-Amyloid Plaques and Neurofibrillary Tangles. Here is a picture of the beta-amyloid plaques and neurofibrillary tangles in Figure 1.

Figure 1. Beta-amyloid plaques and neurofibrillary tangles (Cell death 7mike5000, CC BY-SA 3.0, https://creativecommons.org/licenses/by-sa/3.0 via Wikimedia Commons)
One thing that you will learn from me if you have been around me any length of time is that I like to put things in layman's terms for my patients. Many of them say, "No, the doctor hasn't told me anything about what Alzheimer's disease is." I tell them, "There are little structures in your brain called neurons that almost look like little spiders. The spidery legs communicate with each other but sometimes there is something in between those little spidery legs almost like if you get gum in your hair, and you can't pull it apart. It really gets matted up and there's really nothing you can do to fix it." The "gum in hair" description is how I describe neurofibrillary tangles.
Neurological Changes. Here is what a healthy brain looks like compared to severe Alzheimer's in Figure 2.
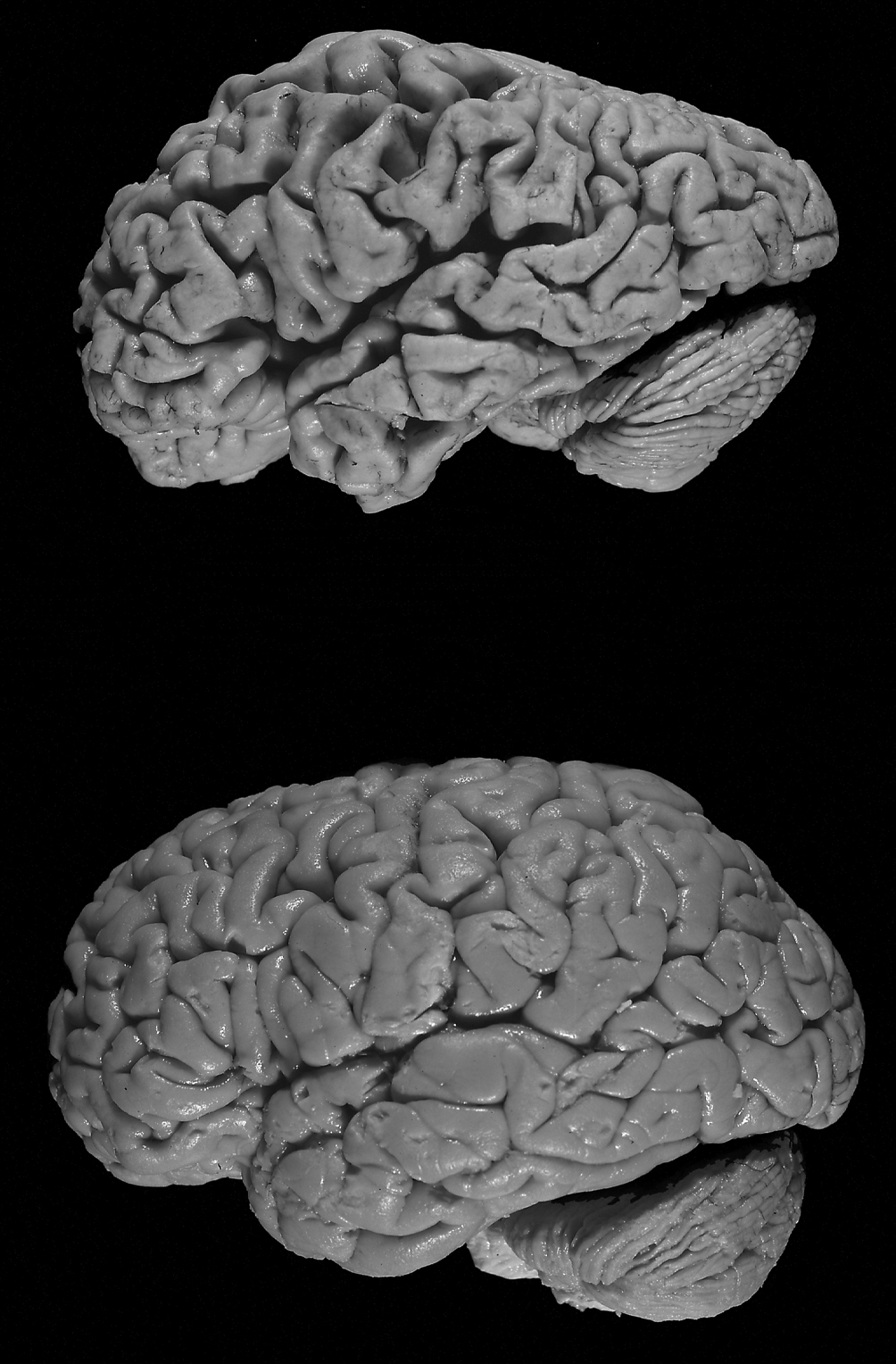
Figure 2. Healthy brain versus a brain with Alzheimer's. (Hersenbank, CC BY-SA 3.0, https://creativecommons.org/licenses/by-sa/3.0, via Wikimedia Commons)
You can see the increased size of the ventricles, and it does look like it is shrinking. In our next several courses, we will go over the neurological changes in each stage of Alzheimer's disease.
Mild Cognitive Impairments (MCI). What about mild cognitive impairment? This is the early at-risk stage where people tend to be either in denial that anything is happening or be overly concerned that something may be occurring. This is when you start seeing those memory changes and language/word-finding changes that are noticeable to others, but the person is still fine living at home. They can still cook, clean, and manage their finances, but things are just getting a little harder. You may see people with a mild cognitive impairment that has a reversible type of dementia that will get better. There may be compensatory activities implemented that can slow the decline, but it is about a 50-50 shot. If a person is diagnosed with MCI, about 50% will end up progressing into Alzheimer's Dementia. The other 50% may be okay. My mother-in-law was in the 50% that was okay. After her NPH and her aneurysm, she was diagnosed with MCI, and thank goodness she was in the 50% who got better.
Diagnosing Dementia
How do we go about diagnosing dementia? It is important to have a family history, brain imaging, blood work, spinal taps, and a mental status exam. We will talk more about some of those exams in the next couple of sessions.
Can Speech-Language Pathologists Diagnose Dementia?
The SLP cannot diagnose dementia. We can conduct mental status or staging assessments to see the level of cognitive decline, but we cannot give the patient a diagnosis of dementia. If we see a patient with the symptoms and the patient does not have that diagnosis, we need to have a good rapport with that MD so that we can request a neuro consult. We describe the symptoms that we see, and we treat the symptoms. We do not treat the disease process. We as SLP's cannot stop Alzheimer's disease, but we can treat the symptoms.
What Might the MD Do?
There are several medications and I have named four of them here for you.
- Aricept (1997) - Most common prescribed of AD medications. One dose is taken at night.
- Reminyl (2001) - Used with vascular and mixed dementia. Once (extended-release) or twice per day doses. Linked to renal and liver issues.
- Exelon (2000) - Adds acetylcholine in the brain. Taken once or twice per day. Titration required and potential for GI problems.
- Namenda (2003) - Regulates glutamate activity (related to learning and memory) Often used as a 2nd drug in a “cocktail” approach to pharmacological treatment
The first three, Aricept, Reminyl, and Exelon are cholinesterase inhibitors (CIs), and they decrease the severity of symptoms caused by dementia because they keep acetylcholine from breaking down. Acetylcholine is key for memory, mood, and new learning. Those medicines are crucial in keeping the acetylcholine present. Namenda is an NMDA receptor antagonist, N-methyl D-aspartate receptor antagonist. This blocks the chemical messenger which is glutamate that is released in excess when damaged by Alzheimer's dementia. This gives some protection but they can be hallucinogenic. They are very similar to some of the anesthetic drugs. Sometimes, patients get a cocktail of a couple of different types. You will see the CIs and the NMDAs used together.
Progression of Impairment
Alzheimer's disease is typically characterized into three stages, early, middle and late, and Alzheimer's is typically a seven to 20-year process. There are many factors that go into this depending on whether a client has the disease long before they are diagnosed. Thus, they may be in those middle stages often before they are even diagnosed.
Stages of Cognitive Impairment
In Part 2, we will be looking at the classifications using the Global Deterioration Scale as well as Allen Cognitive Levels.
Global Deterioration Scale
The Global Deterioration Scale has seven stages. Stage one is a normal adult to stage seven which is late or end-stage dementia. That GDS3 is the mild cognitive impairment that we talked about, and GDS5 is the point where the patient can no longer live independently at home.
- GDS 1 - Normal adult
- GDS 2 - Forgetfulness
- GDS 3 - Early Confusional State
- GDS 4 - Late Confusional State (Mild Dementia)
- GDS 5 - Moderate Dementia
- GDS 6 - Severe Dementia
- GDS 7 - Late/Severe Dementia
Allen Cognitive Levels
Allen Cognitive Levels are going to be used more in the OT profession. The scoring for the Allen Levels is reversed from GDS. If you have a GDS1, you are a normal functioning adult, but the Allen Cognitive Level Six corresponds with GDS1. It is inversely scored and can throw people off.
- 6 Levels (each with 3 components: attention, motor control, verbal performance)
- ACL 0 - Coma
- ACL 1 - Awareness
- ACL 2 - Gross Body Movements
- ACL 3 - Manual Actions
- ACL 4 - Familiar Activity
- ACL 5 - Learning New Activity
- ACL 6 - Planning New Activity
Mental Status Exams
There are many different mental status exams. I have listed many of them for you (see below). Some of these are available online for free, and some you may have to purchase. There are also a few that require certification for you to give them. For example, MOCA is one.
- Brief Cognitive Rating Scale (BCRS)
- Allen Cognitive Level Screen
- ACL Leather Lacing or Placemat Tests
- Clock Drawing Test
- Mini-Mental State Exam
- Functional Assessment Staging (FAST)
- Montreal Cognitive Assessment (MOCA)
- Self-Administered Gerocognitive Exam (SAGE)
- Ross Information Processing Assessment (RIPA)
- Mini-Cog Test
Dementia or Decline?
When we talk about dementia or decline, does it really matter? Does it matter if our patients have an actual dementia diagnosis or not? I am here to tell you that the diagnosis does not change what you do. If there is an existing diagnosis that we see in the medical record, this should send up the red flags. We should look at those patients to see where are they stage-wise and see if there has been a major change in function. We have discussed some of those reversible dementias or red flag conditions that may cause a decline. We may want to evaluate a patient who has those red flag conditions, but it is important to note that we are not treating dementia itself. We are treating the symptoms related to decline and helping the client to develop compensatory strategies. We are using evidence-based treatments in order to help that patient function as high as possible within their level. And in those reversible cases, we may be able to help the client to get back some of that recent decline that occurred. Our therapy enhances neuroplasticity and helps the patient's brain generate new neurons and synapses. We want those dendrites and axons to sprout and be very flexible. We want them to essentially grow and take over for the networks of the brain that have deficits. This is how I explain it to patients. I always tell them brains are a very remarkable thing, and they really are.
Who Should We Evaluate?
Who should we evaluate? Any patients who have signs or symptoms, history of decline, or whose family or staff is reporting a decline in function. We also need to look at patients who have a recent illness or etiology that we know poses a risk.
Can You Slow Decline?
The American Academy of Neurology produced a study in 2009 that suggests that people who are “destined to develop dementia” can delay the onset of accelerated memory decline by doing brain exercises:
- Reading
- Writing
- Crossword Puzzles
- Board Games
- Card Games
- Group discussions
- Music
- Current events recollection
Participants who didn’t do these types of activities lost their memory 3 times as quickly as those who did cognitive exercises 30 minutes a day, 7 days per week.
Next Time (Part 2)
Next time, I will cover the Global Deterioration Scale. We will discuss the stages, cognitive age equivalencies, and the realistic expectations from a therapeutic standpoint.
Questions and Answers
If you see in the chart someone with a brain CT that states there are chronic ischemic changes, is that something that would correspond perhaps to vascular dementia?
Yes, that would be my initial reaction.
Some people are a little bit afraid to discuss Alzheimer's with their doctor because they are afraid that if the diagnosis is dementia, then some nursing homes will not take these individuals. They don't want it on their record so to speak. Do you have any advice for those patients?
I have never encountered in my practice a nursing home that denied a patient because of Alzheimer's diagnosis. I know that certain assisted living facilities will try to look up a patient's stage cognitively because once they are at a certain stage, they require more care. However, I have never actually known a nursing home to deny patient admission due to a specific diagnosis. I sure would hope not. I would be on a soapbox if I heard that.
How long would you wait for spontaneous recovery from a reversible cause before beginning treatment for deficits?
There is research that is out there stating how long spontaneous recovery is for each etiology. For example, after anesthesia, symptoms should resolve in three or four days. For something that is more infectious, you need to wait until that infection is gone and then give at least a few days after that to allow for that spontaneous recovery to occur. The great news is that we are never going to hurt our patients by evaluating them. When in doubt, err on the side of patient well-being.
With the drugs that you discussed that are used to help slow the progression of Alzheimer's, such as Namenda and Aricept, and so forth, do those also work for other types of dementia?
I have not heard of them necessarily being used for other types of dementias. I know several of the types we talked about today do not have any pharmacological intervention. I think most of the research in drugs out there are specifically for Alzheimer's type.
How would we advise patients about lifestyle changes that can also help like exercise and neuroprotective activities?
We will discuss these cognitive stimulation approaches in upcoming talks, but we absolutely should be getting that information out to patients and their families. There is a huge link between physical well-being, physical exercise, and mental acuity.
Here's an example for you of a situation someone has run into. A neurologist completed a mini cognitive test on my dad and said he passed. He told my dad that he was experiencing the normal forgetfulness that happens with aging. What do you suggest we do at this point? Do we get a second opinion or do we try some of the brain stimulation activities and so forth that we were just talking about and check again in six months? What would you do in that situation?
I would definitely really try to do some cognitively stimulating tasks and improve his physical exercise. The more you get your blood pumping, the more oxygen gets to your brain. If you are seeing major signs and symptoms that are interfering with his activities of daily living, as his daughter, I would ask for a second opinion. When in doubt, always get a second opinion.
Citation
Heape, A. (2020). Dementia Diaries Part 1: Understanding the types of dementia. SpeechPathology.com, Article 20393. Retrieved from https://www.speechpathology.com/

