Discussions among audiologists on how to best work with adults with hearing loss usually revolve around pathological or technical issues; for example, how to better understand the physiological aspects of hearing, how to make an accurate diagnosis, or how to optimize the benefits of technology to maximize residual hearing. Although these aspects of audiologic rehabilitation are vitally important, it is additionally helpful to evaluate the impact of interpersonal communication behavior upon communication function and social integration. Communication behavior refers to individual communicative actions that may vary from time to time. Communication function refers to the overall purpose of the collective communication behaviors - namely, social integration.
The simple reason for this additional focus is that communication behavior, whether we hear well or not, has a much more decisive influence upon success or failure in social integration than the simple ability to hear. After all, how we respond to what we hear or perceive is usually the only criteria our communication partners can use to determine how to interact with us. Therefore, an examination of the impact of communication behavior on communication function may be more enlightening as a framework for developing an audiological rehabilitation program than a clinical perspective that considers only pathological or psychological causes of the disabling impact of hearing loss on social integration.
Hearing loss is common, and regardless of the causative factors involved, there are communication behaviors that typically result from it. The inability to hear a conversation clearly as a result of a hearing loss is not much different from being able to hear a conversation but not understand it as a result of a language barrier, as in the case of a non-English speaking immigrant. Neither should be regarded as a psychological or psychosocial disorder. It is helpful to the task of rebuilding a client's communicative confidence to investigate whether the client is using any communication behaviors that could create barriers to successful social integration within his or her culture. This additional clinical focus does not mean that a clinician should deny psychosocial issues caused by hearing loss. It simply suggests that the best foundation for hearing rehabilitation planning is to focus on helping clients restore balance to their communication function.
Two Components of Communication Function
Normal acts of communication involve two components, reception and expression. We receive information about environmental sounds and interpersonal communication through our ears and eyes, and we respond to these stimuli. These responses express our feelings and thoughts and convey messages to others. The resulting interactions determine our effectiveness in interpersonal engagement and social survival. Any impedance to the frequency, quantity, or quality of communication can have a significant impact on the quality and stability of social integration and, if left untreated long enough, a negative impact on mental health. It does not matter whether the impedance is a hearing loss, speech impediment, language barrier, anti-social behavior, or a destructive communication tactic, the result will be the samea negative impact on the ability to engage productively and in healthful ways with other people.
Communication behaviors are culturally derived; they are learned from family and social environments. Hearing is a key determinate of communication behavior as information must first be received accurately in order to learn to respond accurately. Impaired hearing, especially if it is severe and affects the formative years, may impede the ability to adopt expressive communication behavior norms. This interference can be better understood by considering fundamental *attributes of normal communication behavior and how hearing loss can affect those attributes.
The Communication Diet Model
Communication is often called "food for the mind" and is just as necessary to mental health as food is to physical health, so taking a closer look at what happens to the human body when it is deprived of food, can help us to understand what happens to the mind when it is deprived of some of the essential "nutrients" of normal, unhindered communication.
If we neglect to eat an adequate quantity of nutritious food regularly, our bodies become sick unless a correct balance of the essential elements is restored. This is an absolute rule that cannot be ignored without an eventual impact on physical survival. For example, if a person eats regularly, but eats too little or too much, even if their meals are nutritionally well balanced, excessive weight loss or weight gain will result. If a person eats regular, good-sized meals, but eats only junk food devoid of nutritional value, illness will occur. Likewise, a negative effect will happen if a person eats well-balanced, good-sized meals, but skews the frequency by eating too often or too infrequently. Logically then, it should be a reasonable hypothesis that failure to "feed" the mind with an adequate amount of "nutritious" communication at regular intervals, or merely skewing any of the three elements, (regularity, quantity or quality) to one extreme or the other, could trigger the various psychosocial symptoms associated with hearing loss such as loneliness, depression, anxiety, and withdrawal.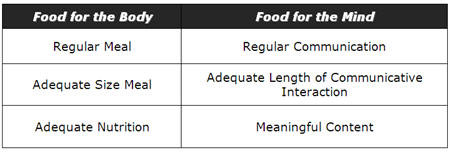
Communication Diet Theory: An Extended Foundation for Hearing Rehabilitation
October 27, 2009
Related Courses
1
https://www.speechpathology.com/slp-ceus/course/ripple-effect-stuttering-community-based-9217
The Ripple Effect of Stuttering: A Community-Based Approach
This is Part 2 of a four-part series. The stuttering experience has a ripple effect that extends far beyond the child who stutters. Parents, teachers, peers, and others must possess both knowledge and skills to best support children who stutter. This course will highlight new clinical tools and resources to provide a community-based treatment approach for stuttering. (Part 1 - Course 9278, Part 3 - Course 9301, Part 4 - Course 9304)
auditory, textual, visual
129
USD
Subscription
Unlimited COURSE Access for $129/year
OnlineOnly
SpeechPathology.com
www.speechpathology.com
The Ripple Effect of Stuttering: A Community-Based Approach
This is Part 2 of a four-part series. The stuttering experience has a ripple effect that extends far beyond the child who stutters. Parents, teachers, peers, and others must possess both knowledge and skills to best support children who stutter. This course will highlight new clinical tools and resources to provide a community-based treatment approach for stuttering. (Part 1 - Course 9278, Part 3 - Course 9301, Part 4 - Course 9304)
9217
Online
PT120M
The Ripple Effect of Stuttering: A Community-Based Approach
Presented by Craig Coleman, MA, CCC-SLP, BCS-F, ASHA Fellow, Mary Weidner, PhD, CCC-SLP
Course: #9217Level: Intermediate2 Hours
ASHA/0.2 Intermediate, Professional; Calif SLPAB/2.0; IACET/0.2; Kansas LTS-S1370/2.0; SAC/2.0
This is Part 2 of a four-part series. The stuttering experience has a ripple effect that extends far beyond the child who stutters. Parents, teachers, peers, and others must possess both knowledge and skills to best support children who stutter. This course will highlight new clinical tools and resources to provide a community-based treatment approach for stuttering. (Part 1 - Course 9278, Part 3 - Course 9301, Part 4 - Course 9304)
2
https://www.speechpathology.com/slp-ceus/course/20q-infection-control-strategies-for-9729
20Q: Infection Control Strategies for SLPs
Speech-language pathologists are expected by policy authorities to apply appropriate measures to protect patients, co-workers and themselves in clinical situations that may expose individuals to infectious microbes. This article provides practical guidelines for implementing infection control principles within the context of the COVID-19 pandemic, including discussion of personal protective equipment (PPE) and disinfecting and cleaning products.
textual, visual
129
USD
Subscription
Unlimited COURSE Access for $129/year
OnlineOnly
SpeechPathology.com
www.speechpathology.com
20Q: Infection Control Strategies for SLPs
Speech-language pathologists are expected by policy authorities to apply appropriate measures to protect patients, co-workers and themselves in clinical situations that may expose individuals to infectious microbes. This article provides practical guidelines for implementing infection control principles within the context of the COVID-19 pandemic, including discussion of personal protective equipment (PPE) and disinfecting and cleaning products.
9729
Online
PT60M
20Q: Infection Control Strategies for SLPs
Presented by A.U. Bankaitis Smith, PhD
Course: #9729Level: Intermediate1 Hour
ASHA/0.1 Intermediate, Professional; Calif SLPAB/1.0; IACET/0.1; Kansas LTS-S1370/1.0; SAC/1.0
Speech-language pathologists are expected by policy authorities to apply appropriate measures to protect patients, co-workers and themselves in clinical situations that may expose individuals to infectious microbes. This article provides practical guidelines for implementing infection control principles within the context of the COVID-19 pandemic, including discussion of personal protective equipment (PPE) and disinfecting and cleaning products.
3
https://www.speechpathology.com/slp-ceus/course/thickened-liquids-in-clinical-practice-10497
Thickened Liquids in Clinical Practice: The Plot “Thickens”
Clinicians who utilize thickened liquids in their clinical practice are aware of their benefits, but what about the risks and contraindications? Advantages and disadvantages of thickened liquids are reviewed in this course with a focus on clinical outcomes, including impacts on medication administration, lung health, and hydration. Product types are evaluated to facilitate appropriate choices for individual clients.
auditory, textual, visual
129
USD
Subscription
Unlimited COURSE Access for $129/year
OnlineOnly
SpeechPathology.com
www.speechpathology.com
Thickened Liquids in Clinical Practice: The Plot “Thickens”
Clinicians who utilize thickened liquids in their clinical practice are aware of their benefits, but what about the risks and contraindications? Advantages and disadvantages of thickened liquids are reviewed in this course with a focus on clinical outcomes, including impacts on medication administration, lung health, and hydration. Product types are evaluated to facilitate appropriate choices for individual clients.
10497
Online
PT60M
Thickened Liquids in Clinical Practice: The Plot “Thickens”
Presented by Angela Mansolillo, MA, CCC-SLP, BCS-S
Course: #10497Level: Intermediate1 Hour
ASHA/0.1 Intermediate, Professional; Calif SLPAB/1.0; IACET/0.1; Kansas LTS-S1370/1.0; SAC/1.0
Clinicians who utilize thickened liquids in their clinical practice are aware of their benefits, but what about the risks and contraindications? Advantages and disadvantages of thickened liquids are reviewed in this course with a focus on clinical outcomes, including impacts on medication administration, lung health, and hydration. Product types are evaluated to facilitate appropriate choices for individual clients.
4
https://www.speechpathology.com/slp-ceus/course/slp-in-nicu-overview-11267
SLP in the NICU: An Overview
This course provides an introductory overview of Speech-Language Pathology services in the Neonatal Intensive Care Unit (NICU), including the unique environment, the SLP’s role, and key components of neonatal care. Topics include cue-based and supportive feeding strategies, instrumental assessments, and approaches for empowering and supporting parents and caregivers.
auditory, textual, visual
129
USD
Subscription
Unlimited COURSE Access for $129/year
OnlineOnly
SpeechPathology.com
www.speechpathology.com
SLP in the NICU: An Overview
This course provides an introductory overview of Speech-Language Pathology services in the Neonatal Intensive Care Unit (NICU), including the unique environment, the SLP’s role, and key components of neonatal care. Topics include cue-based and supportive feeding strategies, instrumental assessments, and approaches for empowering and supporting parents and caregivers.
11267
Online
PT60M
SLP in the NICU: An Overview
Presented by Anna Manilla, MS, CCC-SLP, CLC
Course: #11267Level: Introductory1 Hour
ASHA/0.1 Introductory, Professional; Calif SLPAB/1.0; IACET/0.1; IL EITP/1.0; Kansas LTS-S1370/1.0; SAC/1.0
This course provides an introductory overview of Speech-Language Pathology services in the Neonatal Intensive Care Unit (NICU), including the unique environment, the SLP’s role, and key components of neonatal care. Topics include cue-based and supportive feeding strategies, instrumental assessments, and approaches for empowering and supporting parents and caregivers.
5
https://www.speechpathology.com/slp-ceus/course/dysphagia-in-neurodegenerative-disease-9732
Dysphagia in Neurodegenerative Disease
Dysphagia is common in individuals with amyotrophic lateral sclerosis (ALS) and Parkinson’s disease. This course discusses the underlying pathophysiology and appropriate treatment programs for each disease, as well as use of alternate methods of nutrition/hydration.
auditory, textual, visual
129
USD
Subscription
Unlimited COURSE Access for $129/year
OnlineOnly
SpeechPathology.com
www.speechpathology.com
Dysphagia in Neurodegenerative Disease
Dysphagia is common in individuals with amyotrophic lateral sclerosis (ALS) and Parkinson’s disease. This course discusses the underlying pathophysiology and appropriate treatment programs for each disease, as well as use of alternate methods of nutrition/hydration.
9732
Online
PT60M
Dysphagia in Neurodegenerative Disease
Presented by Debra M. Suiter, PhD, CCC-SLP, BCS-S
Course: #9732Level: Intermediate1 Hour
ASHA/0.1 Intermediate, Professional; Calif SLPAB/1.0; IACET/0.1; Kansas LTS-S1370/1.0; SAC/1.0
Dysphagia is common in individuals with amyotrophic lateral sclerosis (ALS) and Parkinson’s disease. This course discusses the underlying pathophysiology and appropriate treatment programs for each disease, as well as use of alternate methods of nutrition/hydration.
