Introduction
My experience in many facilities, and I hope yours is different than mine, was that mouth care was spotty at best. Many times, we really didn't have mouth care and unfortunately, that seemed to be related to the level of staffing. If you don't have the staff, if you have a skeleton crew, mouth care is one of the very first things they're not going to do. So we need to make sure everybody understands, that puts our patients at risk. There is more to mouth care than just swabbing around the gums or the teeth. And whenever I get lawsuits, they are usually involving something with the dentition, where we didn't clean out the mouth after the patient ate and they choked to death on the residue. It is very important that we deal with mouth care.
Our staff is typically poorly educated. They don't understand the rationale and they don't understand how to do it. Many times when nursing students come into our facilities, they're being taught bad habits and those continue to happen in our facilities.
In this course, we are going to review the importance of mouth care. I will help you formulate talking points to educate your staff. We need to identify how to do mouth care, not only for natural teeth, but for NPO patients and those who has no dentition. I will provide resources that can be utilized to develop a mouth care protocol.
Why Mouth Care?
Why do we need to do oral hygiene? There are many health risks for our patients in addition to the impact of aspiration pneumonia from the bacteria-laden saliva. Mouth care is more than just teeth. We also need to address the tongue. If we only do mouth care on the teeth, the bacteria from the tongue find their way to the teeth almost immediately after we've done mouth care. Later in the course I will provide some mouth care protocols that can be utilized in your facilities.
Concerns
When we look at the chart review, our patients have so many different disease processes, disorders and medications. Those different issues can create a lot of problems with saliva. There are problems with the dentition. Do they have dentures? How well do they fit? Do they have their own teeth? If so, what teeth are still there? Many times, they're missing the premolars and the molars which are important teeth for chewing. When the premolars and molars are missing then the incisors and canines to take over the job of chewing which they're not supposed to do. We also need to look at the condition of the teeth. Sometimes we're better off just taking the teeth out because they're a breeding ground for bacteria.
We also need to review the patient’s medications because that can either create the dry mouth (i.e., xerostomia), or at the other end of the spectrum they can create excess secretions. Patients end up with mouth ulcers, stomatitis and thrush. We also have patients, especially those receiving home healthcare or outpatient services, who are not taking traditional medications. Rather, they are taking “complementary alternative medications (CAM) and we need to make sure those patients understand adding herbs and/or supplements to traditional medications can cause issues. Taking herbs alone can cause mouth sores. So, we need to know what our patients are taking – over-the-counter, herbal supplements, and traditional medications.
Drugs Treating These Conditions Potentially Cause Xerostomia
How many of our patients have these particular disorders in their medical records (Figure 1)?
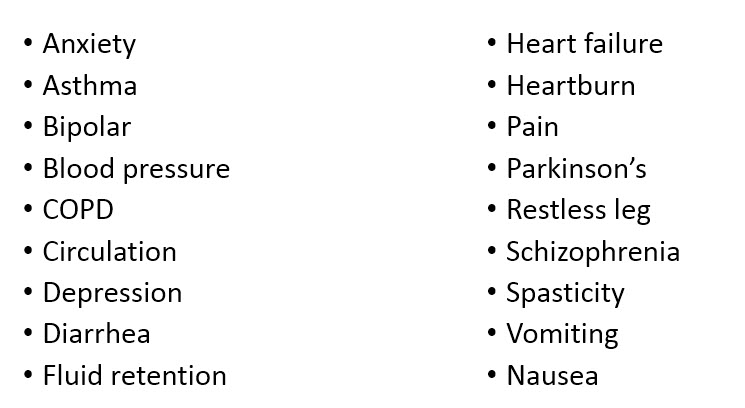
The drugs that are given to patients for these conditions potentially cause dry mouth. So, when reviewing a chart, these are issues that have a lack of saliva production.
When a patient is being treated for anxiety, circulation problems or schizophrenia, the medications that treat those issues often create increased secretions. Then what happens is this domino effect. The doctor writes a prescription for medication to dry up the secretions that were caused by the drugs to treat a condition. There is this continual prescribing of medications.
Patients who have the following conditions are often prescribed medications that cause dysphagia:
- Asthma
- Bipolar
- Blood pressure candidiasis
- Diabetes
- Diarrhea
- Fluid retention
- Fungal infection
- Osteoporosis
So we need to recognize the importance of that medication review. Then we need to look at these particular disorders because the drugs that treat them often cause mouth ulcers, which are going to be extremely painful; thrush, which changes our taste or gives us a bad taste; and esophageal ulcers.
When food is passing through the esophagus, we need to keep in mind the texture and the different tastes. Maybe we need to do bland foods because it irritates the esophageal ulcers. Just because our patients can chew doesn't necessarily mean that they should have texture. Unfortunately, that is what many staff members do not understand. A patient could have strictures, webs, rings, ulcerations, or lesions. When those are present, the food that they consume needs to be very soft and very bland regardless of their ability to chew.
Connection between Occlusion and Human Brain Function
Now I found this bit of information extremely interesting. There is a connection between the teeth and human brain function. In part one (Course XXXX), we talked about needing a minimum of 20 teeth, and they need to be antagonistic pairs. That means the top and the bottom teeth touch. An article by Elsig and colleagues (2015), suggest that mastication should be considered a mild and lifelong daily exercise. Those up-and-down jaw movements for chewing create saliva from the parotid gland that help to form a cohesive bolus. But the researchers also found that this up-and-down movement increases cerebral blood flow. It creates increased oxygen levels and it actually may prevent the decline in brain function because you're improving that chewing function.
Diabetes and Oral Health
There's also a connection with diabetes. Diabetes and dysphagia have a big connection and we often see the diabetic individual having very bad dental health. They end up with periodontitis, which is the inflammatory response to inflamed periodontal tissue. This exacerbates the diabetes and it worsens cardiovascular outcomes. That's very important because it has been found that cardiovascular disease creates arterial damage and changes the size of the olfactory bulb in the brain. So when we're talking about decreased sense of smell, it's not just the regeneration of the neurons in the nasal passages that starts to change the sense of smell, it's changes in the brain. We need to make sure that we're doing very good mouth care because it really does impact the severity of the diabetes and all of the conditions that go with that.
For the diabetic individual, the oral health issues they tend to have include periodontitis, dry mouth (xerostomia), and oral cancer. There is typically a lot of plaque on the mucosa, and you aren’t going to be able to scrape the plaque actually off any of the mucosa. Therefore, really good oral care is a must.
Oral Pathogens and Increased Risk of Esophageal Cancer
It has also been found that there is an abundance of periodontal pathogens in the esophagus that increases or puts a person at a higher risk of esophageal cancer. Mouth care can change everything in our patients, not just aspiration pneumonia. It can change the esophagus, the cell structure and predispose us to esophageal cancer. Research specifically found predictors of increased risk of precancerous lesions include not flossing (I don’t think I have ever seen dental floss in any of my patient's rooms and facilities), a high prevalence of bleeding when probing the gums or brushing the teeth, and elevated colonization of with periodontal pathogens.
Pulpal Necrosis or Pulp Death
Pulp necrosis, or pulp death, can go unrecognized for many patients, especially those who are nonverbal. There will be a low-grade inflammation around the tooth root that can go unnoticed. If the pulp dies, then that changes everything. It is very, very painful. For patients who are nonverbal, they become very aggressive and combative which can be misdiagnosed as a behavioral problem. Then they end up being medicated for a combative behavior. Again, the dental consult can be really important because if it is very painful to chew, then they aren’t going to. Then that creates even more of an issue with frailty.
Oral Health in LTC Facilities
We see problems with oral health in long-term care facilities. It causes widespread malnutrition in the frail elderly because we have the chewing difficulties, the discomfort and the pain. Research shows that there is a connection between fungal infections and denture stomatitis (Scheibler et a., 2017). Denture stomatitis is a very painful mouth ulcer. When that ulceration touches a tooth, it makes you want to cry and chewing is out of the question.
Decayed teeth and bacteria in the saliva actually increase the risk of aspiration pneumonia. There are a lot of studies that suggest that it's not the aspiration of food or liquids, it's the aspiration of bacteria-laden saliva that creates the aspiration pneumonia. This is something we need to pay attention to because how many of our patients have those high-calorie food supplements with a lot of sugar? We're giving that to them to maintain their nutritional status, but it also increases the risk of decay. When we start providing really high sugar supplements, we need to make sure that we're doing mouth care as well. That's a bad combination and therefore it increases the need for mouth care.
When we're looking at our individuals, we need to understand that just because someone isn’t complaining of pain that doesn't mean there isn't a disease going on or an infection. If a patient reports sensitivity to very hot or very cold food items that is a red flag that there could be some dental disease or infections occurring. A person might say that they have very sensitive teeth. Periodontal disease can be present for a number of years and not create any symptoms for the patient. Therefore, don't take a lack of complaining as having a totally healthy mouth because that may not be the case.
Oral Health Care
Providing assistance with mouth care after every meal has been found to reduce the risk of aspiration pneumonia, and actually improves the swallow reflex. Studies have found that when aggressive mouth care is done, that actually increases the sensitivity of the cough reflex. Researchers tracked this at about 30 days after they began mouth care. So there is a connection. Also, if we do frequent professional oral health care and improved hygiene on a daily basis, aspiration pneumonia risk decreases by 40% in high-risk individuals. Professional oral health care means a dentist or a dental hygienist. It is not the nursing staff. Many studies have discussed the need for these professionals to come into our facilities on a regular basis to work with clients. In the facilities where I have worked, I can't tell you when I've ever seen a dental consult or a dentist or hygienist come into the facility. It's very difficult to take these individuals out to see a dentist so it usually isn't done. Hopefully, your experience is different.
Proper oral health can improve the cough reflex. Poor oral health impacts taste. A person cannot taste anything if there is crust on the tongue. It doesn’t take a long time for crust to build up on the tongue. I see some clients several times a week and within two days there's crust on the tongue. Within one day there can be crust on the tongue because the saliva is so viscous and there's no mouth care. We need to be very careful when cleaning the tongue.
Bacterial growth changes how things taste, and patients complain about taste all the time. Everything tastes the same or it has no taste to it which then creates problems with eating because it's not pleasurable. So they stop eating.
Variables Influencing Risk of Aspiration Pneumonia Directly
Factors or variables that influence aspiration pneumonia directly are low levels of salivary substance P. Salivary substance P is a muscle stimulant that helps with the swallow. A number of years ago there were some studies done in Tokyo looking at Parkinson's patients and stroke patients. What they found is not only did patients have dysphagia but they had low levels of substance P. When they did a particular treatment, the substance P increased and swallowing improved as well. Some doctors are prescribing ACE inhibitors not for their normal usage but to increase the levels of substance P. ACE inhibitors often make you cough and when the cough response improves, the patient may be able to cough and clear. If a person’s cough reflex sensitivity is very low, they are not going to be able to trigger that cough.
It has also been found that oropharyngeal pathogens are very high in elderly individuals. So it’s very important to take a look at all those factors as well.
Good oral health is dependent on good plaque removal which can’t be done with a Toothette swab. Good oral health also relies on a low sugar diet and adequate saliva flow. Usually in facilities, we see the exact opposite. Patients don't have good plaque removal, they don't have good saliva flow and they have a very high sugar diet because they crave sweets. That's what they taste. So we see a complete opposite of what oral health relies on.
With patients who may be able to do their own dental care, good plaque control relies on fine motor skills, adequate vision, and patient motivation. A person in your facility may have adequate motor skills and they can see adequately, but they're not motivated. Two out of three doesn't make it. They need all three factors.
Plaque
Plaque is that sticky layer of bacteria. Interestingly, within minutes of brushing the teeth, plaque starts to come back. It doesn't stay away for very long. Plaque is even present in patients who are NPO because their mouth is stagnant, and they don't have good mouth care.
When plaque hardens it turns into tartar or calculus. The only way to remove that is with the scaling instruments at the dentist's office which is a painful process. For many elderly individuals, it may require sedation and they don't do well with that. It is suggested that mouth care should be done twice a day, and that should in the care plan.
Tooth Loss and Oral Function
When there is tooth loss, many times the patient’s diet is downgraded because they no longer have 20 teeth or 13 teeth. It’s possible that they only have the incisors and canines, if that. Then, they are put on a very soft diet that does not stimulate saliva production because they no longer have to chew.
Also, when foods are pureed, the nutrient density is reduced because addition liquids have been added. The food is not as nutritious as it was in its original form and the individual has to eat much more of this energy-diluted food to meet their needs. Usually, they're barely eating enough to begin with and then malnutrition starts to occur.

